An insulin pump is a medical device used for the administration of insulin in the treatment of diabetes mellitus, also known as continuous subcutaneous insulin therapy. The device configuration may vary depending on design. A traditional pump includes:
Intensive insulin therapy or flexible insulin therapy is a therapeutic regimen for diabetes mellitus treatment. This newer approach contrasts with conventional insulin therapy. Rather than minimize the number of insulin injections per day, the intensive approach favors flexible meal times with variable carbohydrate as well as flexible physical activities. The trade-off is the increase from 2 or 3 injections per day to 4 or more injections per day, which was considered "intensive" relative to the older approach. In North America in 2004, many endocrinologists prefer the term "flexible insulin therapy" (FIT) to "intensive therapy" and use it to refer to any method of replacing insulin that attempts to mimic the pattern of small continuous basal insulin secretion of a working pancreas combined with larger insulin secretions at mealtimes. The semantic distinction reflects changing treatment.
The following is a glossary of diabetes which explains terms connected with diabetes.

Blood glucose monitoring is the use of a glucose meter for testing the concentration of glucose in the blood (glycemia). Particularly important in diabetes management, a blood glucose test is typically performed by piercing the skin to draw blood, then applying the blood to a chemically active disposable 'test-strip'. Different manufacturers use different technology, but most systems measure an electrical characteristic and use this to determine the glucose level in the blood. The test is usually referred to as capillary blood glucose.
Drugs used in diabetes treat diabetes mellitus by altering the glucose level in the blood. With the exceptions of insulin, most GLP receptor agonists, and pramlintide, all are administered orally and are thus also called oral hypoglycemic agents or oral antihyperglycemic agents. There are different classes of anti-diabetic drugs, and their selection depends on the nature of the diabetes, age and situation of the person, as well as other factors.
Diabetes mellitus is a chronic disease in cats whereby either insufficient insulin response or insulin resistance leads to persistently high blood glucose concentrations. Diabetes affects up to 1 in 230 cats, and may be becoming increasingly common. Diabetes mellitus is less common in cats than in dogs. Eighty to ninety-five percent of diabetic cats experience something similar to type 2 diabetes but are generally severely insulin dependent by the time symptoms are diagnosed. The condition is treatable, and if treated properly the cat can experience a normal life expectancy. In type 2 cats, prompt effective treatment may lead to diabetic remission, in which the cat no longer needs injected insulin. Untreated, the condition leads to increasingly weak legs in cats and eventually to malnutrition, ketoacidosis and/or dehydration, and death.

Diabetic hypoglycemia is a low blood glucose level occurring in a person with diabetes mellitus. It is one of the most common types of hypoglycemia seen in emergency departments and hospitals. According to the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP), and based on a sample examined between 2004 and 2005, an estimated 55,819 cases involved insulin, and severe hypoglycemia is likely the single most common event.
Stress hyperglycemia is a medical term referring to transient elevation of the blood glucose due to the stress of illness. It usually resolves spontaneously, but must be distinguished from various forms of diabetes mellitus.

Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that originates when very little or no insulin is produced by the islets of Langerhans in the pancreas. Insulin is a hormone required for the cells to use blood sugar for energy and it helps regulate normal glucose levels in the bloodstream. Before treatment this results in high blood sugar levels in the body. The common symptoms of this elevated blood sugar are frequent urination, increased thirst, increased hunger, weight loss, and other serious complications. Additional symptoms may include blurry vision, tiredness, and slow wound healing. Symptoms typically develop over a short period of time, often a matter of weeks.
The term diabetes includes several different metabolic disorders that all, if left untreated, result in abnormally high concentration of a sugar called glucose in the blood. Diabetes mellitus type 1 results when the pancreas no longer produces significant amounts of the hormone insulin, usually owing to the autoimmune destruction of the insulin-producing beta cells of the pancreas. Diabetes mellitus type 2, in contrast, is now thought to result from autoimmune attacks on the pancreas and/or insulin resistance. The pancreas of a person with type 2 diabetes may be producing normal or even abnormally large amounts of insulin. Other forms of diabetes mellitus, such as the various forms of maturity onset diabetes of the young, may represent some combination of insufficient insulin production and insulin resistance. Some degree of insulin resistance may also be present in a person with type 1 diabetes.
An insulin analog is any of several types of insulin (medication) that are altered forms of the hormone insulin, different from any occurring in nature, but still available to the human body for performing the same action as human insulin in terms of controlling blood glucose levels in diabetes. Through genetic engineering of the underlying DNA, the amino acid sequence of insulin can be changed to alter its ADME characteristics. Officially, the U.S. Food and Drug Administration (FDA) refers to these agents as insulin receptor ligands, although they are usually just referred to as insulin analogs.
Pulsatile intravenous insulin therapy, sometimes called metabolic activation therapy or cellular activation therapy, describes in a literal sense the intravenous injection of insulin in pulses versus continuous infusions. Injection of insulin in pulses mimics the physiological secretions of insulin by the pancreas into the portal vein which then drains into the liver. In healthy, non-diabetic individuals, pancreatic secretions of insulin correspond to the intake of food. The pancreas will secrete variable amounts of insulin based upon the amount of food consumed among other factors. Continuous exposure to insulin and glucagon is known to decrease the hormones' metabolic effectiveness on glucose production in humans due to the body developing an increased tolerance to the hormones. Down-regulation at the cellular level may partially explain the decreased action of steady-state levels of insulin, while pulsatile hormone secretion may allow recovery of receptor affinity and numbers for insulin. Intermittent intravenous insulin administration with peaks of insulin concentrations may enhance suppression of gluconeogenesis and reduce hepatic glucose production.
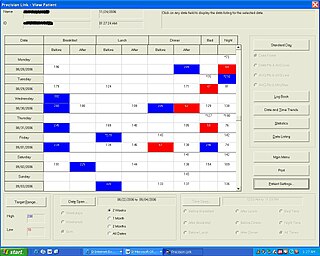
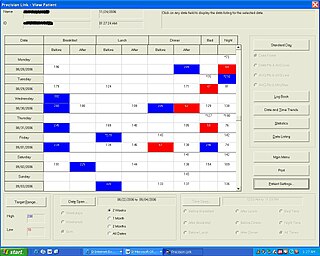
Diabetes Management Software refers to software tools that run on personal computers and personal digital assistants to help persons with Type 1 and Type 2 diabetes manage the data associated with:
Chronic Somogyi rebound is a contested explanation of phenomena of elevated blood sugars in the morning. Also called the Somogyi effect and posthypoglycemic hyperglycemia, it is a rebounding high blood sugar that is a response to low blood sugar. When managing the blood glucose level with insulin injections, this effect is counter-intuitive to people who experience high blood sugar in the morning as a result of an overabundance of insulin at night.

Insulin aspart, sold under the brand name NovoLog and Fiasp, among others, is a type of manufactured insulin used to treat type 1 and type 2 diabetes. It is generally used by injection under the skin but may also be used by injection into a vein. Maximum effect occurs after about 1–3 hours and lasts for 3–5 hours. Generally a longer-acting insulin like insulin NPH is also needed.

Regular insulin, also known as neutral insulin and soluble insulin, is a type of short-acting insulin. It is used to treat type 1 diabetes, type 2 diabetes, gestational diabetes, and complications of diabetes such as diabetic ketoacidosis and hyperosmolar hyperglycemic states. It is also used along with glucose to treat high blood potassium levels. Typically it is given by injection under the skin, but may also be used by injection into a vein or muscle. Onset of effect is typically in 30 minutes and it typically lasts for 8 hours.

As a medication, insulin is any pharmaceutical preparation of the protein hormone insulin that is used to treat high blood glucose. Such conditions include type 1 diabetes, type 2 diabetes, gestational diabetes, and complications of diabetes such as diabetic ketoacidosis and hyperosmolar hyperglycemic states. Insulin is also used along with glucose to treat hyperkalemia. Typically it is given by injection under the skin, but some forms may also be used by injection into a vein or muscle. There are various types of insulin, suitable for various time spans. The types are often all called insulin in the broad sense, although in a more precise sense, insulin is identical to the naturally occurring molecule whereas insulin analogues have slightly different molecules that allow for modified time of action. It is on the World Health Organization's List of Essential Medicines. In 2019, regular human insulin was the 298th most commonly prescribed medication in the United States, with more than 1 million prescriptions.

MiniMed Paradigm is a series of insulin pumps manufactured by Medtronic for patients with diabetes mellitus. The pump operates with a single AAA battery and uses a piston-plunger pump to infuse a programmed amount of insulin into the patient through a length of tubing. The Paradigm uses a one-way wireless radio frequency link to receive blood sugar measurements from select glucose meters. The Paradigm RT series adds the ability to receive data from a mated continuous blood-glucose monitor. Although the pump can use these measurements to assist in calculating a dose of insulin, no actual change in insulin delivery occurs without manual user-intervention.
Neonatal diabetes mellitus (NDM) is a disease that affects an infant and their body's ability to produce or use insulin. NDM is a monogenic form of diabetes that occurs in the first 6 months of life. Infants do not produce enough insulin, leading to an increase in glucose accumulation. It is a rare disease, occurring in only one in 100,000 to 500,000 live births. NDM can be mistaken for the much more common type 1 diabetes, but type 1 diabetes usually occurs later than the first 6 months of life. There are two types of NDM: permanent neonatal diabetes mellitus (PNDM) is a lifelong condition. Transient neonatal diabetes mellitus (TNDM) is diabetes that disappears during the infant stage but may reappear later in life.

Insulin degludec (INN/USAN) is an ultralong-acting basal insulin analogue that was developed by Novo Nordisk under the brand name Tresiba. It is administered via subcutaneous injection once daily to help control the blood sugar level of those with diabetes. It has a duration of action that lasts up to 42 hours, making it a once-daily basal insulin, that is one that provides a base insulin level, as opposed to the fast- and short-acting bolus insulins.