Gangrene is a type of tissue death caused by a lack of blood supply. Symptoms may include a change in skin color to red or black, numbness, swelling, pain, skin breakdown, and coolness. The feet and hands are most commonly affected. If the gangrene is caused by an infectious agent, it may present with a fever or sepsis.

An ulcer is a sore on the skin or a mucous membrane, accompanied by the disintegration of tissue. Ulcers can result in complete loss of the epidermis and often portions of the dermis and even subcutaneous fat. Ulcers are most common on the skin of the lower extremities and in the gastrointestinal tract. An ulcer that appears on the skin is often visible as an inflamed tissue with an area of reddened skin. A skin ulcer is often visible in the event of exposure to heat or cold, irritation, or a problem with blood circulation.
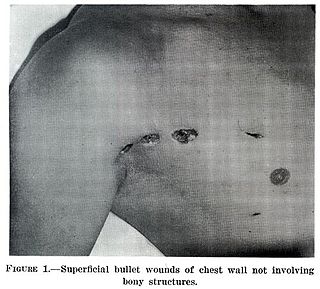
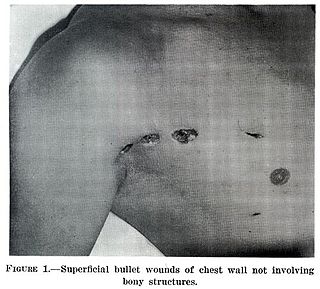
A wound is a rapid onset of injury that involves lacerated or punctured skin, or a contusion from blunt force trauma or compression. In pathology, a wound is an acute injury that damages the epidermis of the skin. To heal a wound, the body undertakes a series of actions collectively known as the wound healing process.

Peripheral artery disease (PAD) is an abnormal narrowing of arteries other than those that supply the heart or brain. PAD can happen in any blood vessel, but it is more common in the legs than the arms.
Diabetic neuropathy is various types of nerve damage associated with diabetes mellitus. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from a microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.

Peripheral neuropathy, often shortened to neuropathy, is a general term describing damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerves are affected. Neuropathy affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.
A complication in medicine, or medical complication, is an unfavorable result of a disease, health condition, or treatment. Complications may adversely affect the prognosis, or outcome, of a disease. Complications generally involve a worsening in the severity of the disease or the development of new signs, symptoms, or pathological changes that may become widespread throughout the body and affect other organ systems. Thus, complications may lead to the development of new diseases resulting from previously existing diseases. Complications may also arise as a result of various treatments.

Neuropathic arthropathy, also known as Charcot joint after the first to describe it, Jean-Martin Charcot, refers to progressive degeneration of a weight-bearing joint, a process marked by bony destruction, bone resorption, and eventual deformity due to loss of sensation. Onset is usually insidious.
The term diabetes includes several different metabolic disorders that all, if left untreated, result in abnormally high concentrations of a sugar called glucose in the blood. Diabetes mellitus type 1 results when the pancreas no longer produces significant amounts of the hormone insulin, usually owing to the autoimmune destruction of the insulin-producing beta cells of the pancreas. Diabetes mellitus type 2, in contrast, is now thought to result from autoimmune attacks on the pancreas and/or insulin resistance. The pancreas of a person with type 2 diabetes may be producing normal or even abnormally large amounts of insulin. Other forms of diabetes mellitus, such as the various forms of maturity-onset diabetes of the young, may represent some combination of insufficient insulin production and insulin resistance. Some degree of insulin resistance may also be present in a person with type 1 diabetes.

Venous ulcer is defined by the American Venous Forum as "a full-thickness defect of skin, most frequently in the ankle region, that fails to heal spontaneously and is sustained by chronic venous disease, based on venous duplex ultrasound testing." Venous ulcers are wounds that are thought to occur due to improper functioning of venous valves, usually of the legs. They are an important cause of chronic wounds, affecting 1% of the population. Venous ulcers develop mostly along the medial distal leg, and can be painful with negative effects on quality of life.
A chronic wound is a wound that does not heal in an orderly set of stages and in a predictable amount of time the way most wounds do; wounds that do not heal within three months are often considered chronic. Chronic wounds seem to be detained in one or more of the phases of wound healing. For example, chronic wounds often remain in the inflammatory stage for too long. To overcome that stage and jump-start the healing process, a number of factors need to be addressed such as bacterial burden, necrotic tissue, and moisture balance of the whole wound. In acute wounds, there is a precise balance between production and degradation of molecules such as collagen; in chronic wounds this balance is lost and degradation plays too large a role.

Diabetic shoes are specially designed shoes, or shoe inserts, intended to reduce the risk of skin breakdown in diabetics with existing foot disease and relieve pressure to prevent diabetic foot ulcers.

David G. Armstrong is an American podiatric surgeon and researcher most widely known for his work in amputation prevention, the diabetic foot, and wound healing. He and his frequent collaborators, Lawrence A. Lavery and Andrew J.M. Boulton, have together produced many key works in the taxonomy, classification and treatment of the diabetic foot. He is Professor of Surgery with Tenure and director of the Southwestern Academic Limb Salvage Alliance (SALSA) at the Keck School of Medicine of the University of Southern California and has produced more than 650 peer reviewed manuscripts and more than 110 book chapters.

Arterial insufficiency ulcers are mostly located on the lateral surface of the ankle or the distal digits. They are commonly caused by peripheral artery disease (PAD).
Complications of diabetes are secondary diseases that are a result of elevated blood glucose levels that occur in diabetic patients. These complications can be divided into two types: acute and chronic. Acute complications are complications that develop rapidly and can be exemplified as diabetic ketoacidosis (DKA), hyperglycemic hyperosmolar state (HHS), lactic acidosis (LA), and hypoglycemia. Chronic complications develop over time and are generally classified in two categories: microvascular and macrovascular. Microvascular complications include neuropathy, nephropathy, and retinopathy; while cardiovascular disease, stroke, and peripheral vascular disease are included in the macrovascular complications.
Hereditary sensory and autonomic neuropathy type I or hereditary sensory neuropathy type I is a group of autosomal dominant inherited neurological diseases that affect the peripheral nervous system particularly on the sensory and autonomic functions. The hallmark of the disease is the marked loss of pain and temperature sensation in the distal parts of the lower limbs. The autonomic disturbances, if present, manifest as sweating abnormalities.

Diabetic foot ulcer is a breakdown of the skin and sometimes deeper tissues of the foot that leads to sore formation. It may occur due to a variety of mechanisms. It is thought to occur due to abnormal pressure or mechanical stress chronically applied to the foot, usually with concomitant predisposing conditions such as peripheral sensory neuropathy, peripheral motor neuropathy, autonomic neuropathy or peripheral arterial disease. It is a major complication of diabetes mellitus, and it is a type of diabetic foot disease. Secondary complications to the ulcer, such as infection of the skin or subcutaneous tissue, bone infection, gangrene or sepsis are possible, often leading to amputation.
Total contact casting (TCC) is a specially designed cast designed to take weight off of the foot (off-loading) in patients with diabetic foot ulcers (DFUs). Reducing pressure on the wound by taking weight off the foot has proven to be very effective in DFU treatment. DFUs are a major factor leading to lower leg amputations among the diabetic population in the US with 85% of amputations in diabetics being preceded by a DFU. Furthermore, the five-year post-amputation mortality rate among diabetics is estimated at 45% for those with neuropathic DFUs.
Electrochemical skin conductance (ESC) is an objective, non-invasive and quantitative electrophysiological measure of skin conductance through the application of a pulsating direct current on the skin. It is based on reverse iontophoresis and steady chronoamperometry. ESC is intended to provide insight into and assess sudomotor function and small fiber peripheral neuropathy. The measure was principally developed by Impeto Medical to diagnose cystic fibrosis from historical research at the Mayo Clinic and then tested on others diseases with peripheral neuropathic alterations in general. It was later integrated into health connected scales by Withings.

Diabetic foot infection is any infection of the foot in a diabetic person. The most frequent cause of hospitalization for diabetic patients is due to foot infections. Symptoms may include pus from a wound, redness, swelling, pain, warmth, tachycardia, or tachypnea. Complications can include infection of the bone, tissue death, amputation, or sepsis. They are common and occur equally frequently in males and females. Older people are more commonly affected.