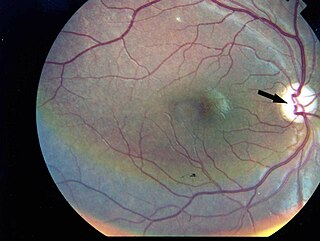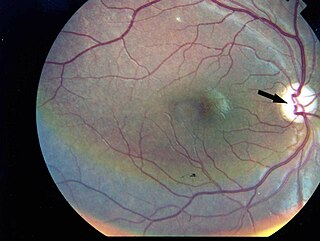
Wolfram syndrome, also called DIDMOAD, is a rare autosomal-recessive genetic disorder that causes childhood-onset diabetes mellitus, optic atrophy, and deafness as well as various other possible disorders including neurodegeneration.
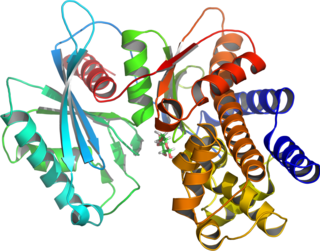
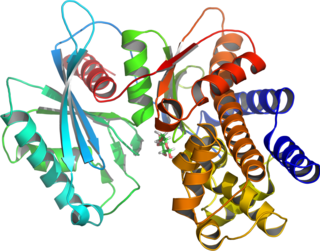
Glucokinase is an enzyme that facilitates phosphorylation of glucose to glucose-6-phosphate. Glucokinase occurs in cells in the liver and pancreas of humans and most other vertebrates. In each of these organs it plays an important role in the regulation of carbohydrate metabolism by acting as a glucose sensor, triggering shifts in metabolism or cell function in response to rising or falling levels of glucose, such as occur after a meal or when fasting. Mutations of the gene for this enzyme can cause unusual forms of diabetes or hypoglycemia.
Maturity-onset diabetes of the young (MODY) refers to any of several hereditary forms of diabetes mellitus caused by mutations in an autosomal dominant gene disrupting insulin production. Along with neonatal diabetes, MODY is a form of the conditions known as monogenic diabetes. While the more common types of diabetes involve more complex combinations of causes involving multiple genes and environmental factors, each forms of MODY are caused by changes to a single gene (monogenic). GCK-MODY and HNF1A-MODY are the most common forms.
Pancreatic diseases are diseases that affect the pancreas, an organ in most vertebrates and in humans and other mammals located in the abdomen. The pancreas plays a role in the digestive and endocrine system, producing enzymes which aid the digestion process and the hormone insulin, which regulates blood sugar levels. The most common pancreatic disease is pancreatitis, an inflammation of the pancreas which could come in acute or chronic form. Other pancreatic diseases include diabetes mellitus, exocrine pancreatic insufficiency, cystic fibrosis, pseudocysts, cysts, congenital malformations, tumors including pancreatic cancer, and hemosuccus pancreaticus.
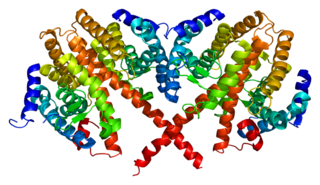
Hepatocyte nuclear factors (HNFs) are a group of phylogenetically unrelated transcription factors that regulate the transcription of a diverse group of genes into proteins. These proteins include blood clotting factors and in addition, enzymes and transporters involved with glucose, cholesterol, and fatty acid transport and metabolism.
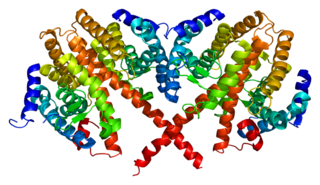
Hepatocyte nuclear factor 4 alpha (HNF4A) also known as NR2A1 is a nuclear receptor that in humans is encoded by the HNF4A gene.

PDX1, also known as insulin promoter factor 1, is a transcription factor in the ParaHox gene cluster. In vertebrates, Pdx1 is necessary for pancreatic development, including β-cell maturation, and duodenal differentiation. In humans this protein is encoded by the PDX1 gene, which was formerly known as IPF1. The gene was originally identified in the clawed frog Xenopus laevis and is present widely across the evolutionary diversity of bilaterian animals, although it has been lost in evolution in arthropods and nematodes. Despite the gene name being Pdx1, there is no Pdx2 gene in most animals; single-copy Pdx1 orthologs have been identified in all mammals. Coelacanth and cartilaginous fish are, so far, the only vertebrates shown to have two Pdx genes, Pdx1 and Pdx2.

Neurogenic differentiation 1 (Neurod1), also called β2, is a transcription factor of the NeuroD-type. It is encoded by the human gene NEUROD1.

Transcription factor MafA is a protein that in humans is encoded by the MAFA gene. It is a member of the Maf family of transcription factors.

Wolcott–Rallison syndrome,WRS, is a rare, autosomal recessive disorder with infancy-onset diabetes mellitus, multiple epiphyseal dysplasia, osteopenia, mental retardation or developmental delay, and hepatic and renal dysfunction as main clinical findings. Patients with WRS have mutations in the EIF2AK3 gene, which encodes the eukaryotic translation initiation factor 2-alpha kinase 3. Other disease names include multiple epiphyseal dysplasia and early-onset diabetes mellitus. Most patients with this disease do not survive to adulthood. The majority of WRS patients die from fulminant hepatitis during childhood. There are few reported cases for this disease. Of the 54 families worldwide with reported WRS cases, 22.2% of them are from the Kingdom of Saudi Arabia. Of the 23 WRS patients in Saudi Arabia, all but one is the result of consanguineous marriages. Another country where WRS cases have been found is Kosovo. Here, the Albanian population is also known for consanguineous marriages, but there were some cases involving patients from non-consanguineous parents that were carriers for the same mutant allele.

MODY 1 or HNF4A-MODY is a form of maturity onset diabetes of the young.
MODY 2 or GCK-MODY is a form of maturity-onset diabetes of the young. It is due to any of several mutations in the GCK gene on human chromosome 7 for glucokinase. Glucokinase serves as the glucose sensor for the pancreatic beta cell. Normal glucokinase triggers insulin secretion as the glucose exceeds about 90 mg/dl. These loss-of-function mutations result in a glucokinase molecule that is less sensitive or less responsive to rising levels of glucose. The beta cells in MODY 2 have a normal ability to make and secrete insulin, but do so only above an abnormally high threshold. This produces a chronic, mild increase in blood sugar, which is usually asymptomatic. It is usually detected by accidental discovery of mildly elevated blood sugar. An oral glucose tolerance test is much less abnormal than would be expected from the impaired (elevated) fasting blood sugar, since insulin secretion is usually normal once the glucose has exceeded the threshold for that specific variant of the glucokinase enzyme.
MODY 3 or HNF1A-MODY is a form of maturity-onset diabetes of the young. It is caused by mutations of the HNF1-alpha gene, a homeobox gene on human chromosome 12. This is the most common type of MODY in populations with European ancestry, accounting for about 70% of all cases in Europe. HNF1α is a transcription factor that is thought to control a regulatory network important for differentiation of beta cells. Mutations of this gene lead to reduced beta cell mass or impaired function. MODY 1 and MODY 3 diabetes are clinically similar. About 70% of people develop this type of diabetes by age 25 years, but it occurs at much later ages in a few. This type of diabetes can often be treated with sulfonylureas with excellent results for decades. However, the loss of insulin secretory capacity is slowly progressive and most eventually need insulin.

Renal cysts and diabetes syndrome (RCAD), also known as MODY 5 or HNF1B-MODY, is a form of maturity onset diabetes of the young.
Permanent neonatal diabetes mellitus (PNDM) is a newly identified and potentially treatable form of monogenic diabetes. This type of neonatal diabetes is caused by activating mutations of the KCNJ11 gene, which codes for the Kir6.2 subunit of the beta cell KATP channel. This disease is considered to be a type of maturity onset diabetes of the young (MODY).

Transient neonatal diabetes mellitus (TNDM) is a form of neonatal diabetes presenting at birth that is not permanent. This disease is considered to be a type of maturity onset diabetes of the young (MODY).

Neonatal diabetes mellitus (NDM) is a disease that affects an infant and their body's ability to produce or use insulin.NDM is a kind of diabetes that is monogenic and arises in the first 6 months of life. Infants do not produce enough insulin, leading to an increase in glucose accumulation. It is a rare disease, occurring in only one in 100,000 to 500,000 live births. NDM can be mistaken for the much more common type 1 diabetes, but type 1 diabetes usually occurs later than the first 6 months of life. There are two types of NDM: permanent neonatal diabetes mellitus (PNDM), a lifelong condition, and transient neonatal diabetes mellitus (TNDM), a form of diabetes that disappears during the infant stage but may reappear later in life.
MODY 6 or NEUROD1-MODY is a form of maturity onset diabetes of the young.

Neurogenin-3 (NGN3) is a protein that in humans is encoded by the Neurog3 gene.

Pancreatic progenitor cells are multipotent stem cells originating from the developing fore-gut endoderm which have the ability to differentiate into the lineage specific progenitors responsible for the developing pancreas.