Related Research Articles
Diffusing capacity of the lung (DL) measures the transfer of gas from air in the lung, to the red blood cells in lung blood vessels. It is part of a comprehensive series of pulmonary function tests to determine the overall ability of the lung to transport gas into and out of the blood. DL, especially DLCO, is reduced in certain diseases of the lung and heart. DLCO measurement has been standardized according to a position paper by a task force of the European Respiratory and American Thoracic Societies.

Pulmonary edema, also known as pulmonary congestion, is excessive liquid accumulation in the tissue and air spaces of the lungs. It leads to impaired gas exchange and may cause hypoxemia and respiratory failure. It is due to either failure of the left ventricle of the heart to remove oxygenated blood adequately from the pulmonary circulation, or an injury to the lung tissue directly or blood vessels of the lung.

A pulmonary artery is an artery in the pulmonary circulation that carries deoxygenated blood from the right side of the heart to the lungs. The largest pulmonary artery is the main pulmonary artery or pulmonary trunk from the heart, and the smallest ones are the arterioles, which lead to the capillaries that surround the pulmonary alveoli.

Pulmonary hypertension is a condition of increased blood pressure in the arteries of the lungs. Symptoms include shortness of breath, fainting, tiredness, chest pain, swelling of the legs, and a fast heartbeat. The condition may make it difficult to exercise. Onset is typically gradual. According to the definition at the 6th World Symposium of Pulmonary Hypertension in 2018, a patient is deemed to have pulmonary hypertension if the pulmonary mean arterial pressure is greater than 20mmHg at rest, revised down from a purely arbitrary 25mmHg, and pulmonary vascular resistance (PVR) greater than 3 Wood units.

Pulmonary alveolar proteinosis (PAP) is a rare lung disorder characterized by an abnormal accumulation of surfactant-derived lipoprotein compounds within the alveoli of the lung. The accumulated substances interfere with the normal gas exchange and expansion of the lungs, ultimately leading to difficulty breathing and a predisposition to developing lung infections. The causes of PAP may be grouped into primary, secondary, and congenital causes, although the most common cause is a primary autoimmune condition in an individual.

Eisenmenger syndrome or Eisenmenger's syndrome is defined as the process in which a long-standing left-to-right cardiac shunt caused by a congenital heart defect causes pulmonary hypertension and eventual reversal of the shunt into a cyanotic right-to-left shunt. Because of the advent of fetal screening with echocardiography early in life, the incidence of heart defects progressing to Eisenmenger syndrome has decreased.

Atelectasis is the collapse or closure of a lung resulting in reduced or absent gas exchange. It is usually unilateral, affecting part or all of one lung. It is a condition where the alveoli are deflated down to little or no volume, as distinct from pulmonary consolidation, in which they are filled with liquid. It is often called a collapsed lung, although that term may also refer to pneumothorax.

Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

Transposition of the great vessels (TGV) is a group of congenital heart defects involving an abnormal spatial arrangement of any of the great vessels: superior and/or inferior venae cavae, pulmonary artery, pulmonary veins, and aorta. Congenital heart diseases involving only the primary arteries belong to a sub-group called transposition of the great arteries (TGA), which is considered the most common congenital heart lesion that presents in neonates.
Pulmonary hemorrhage is an acute bleeding from the lung, from the upper respiratory tract and the trachea, and the pulmonary alveoli. When evident clinically, the condition is usually massive. The onset of pulmonary hemorrhage is characterized by a cough productive of blood (hemoptysis) and worsening of oxygenation leading to cyanosis. Treatment should be immediate and should include tracheal suction, oxygen, positive pressure ventilation, and correction of underlying abnormalities such as disorders of coagulation. A blood transfusion may be necessary.

Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.
Cardiac asthma is the medical condition of intermittent wheezing, coughing, and shortness of breath that is associated with underlying congestive heart failure (CHF). Symptoms of cardiac asthma are related to the heart's inability to effectively and efficiently pump blood in a CHF patient. This can lead to accumulation of fluid in and around the lungs, disrupting the lung's ability to oxygenate blood.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.
A right-to-left shunt is a cardiac shunt which allows blood to flow from the right heart to the left heart. This terminology is used both for the abnormal state in humans and for normal physiological shunts in reptiles.
A pulmonary shunt is the passage of deoxygenated blood from the right side of the heart to the left without participation in gas exchange in the pulmonary capillaries. It is a pathological condition that results when the alveoli of parts of the lungs are perfused with blood as normal, but ventilation fails to supply the perfused region. In other words, the ventilation/perfusion ratio of those areas is zero.
The Alveolar–arterial gradient, is a measure of the difference between the alveolar concentration (A) of oxygen and the arterial (a) concentration of oxygen. It is a useful parameter for narrowing the differential diagnosis of hypoxemia.
Swimming induced pulmonary edema (SIPE), also known as immersion pulmonary edema, is a life threatening condition that occurs when fluids from the blood leak abnormally from the small vessels of the lung (pulmonary capillaries) into the airspaces (alveoli).

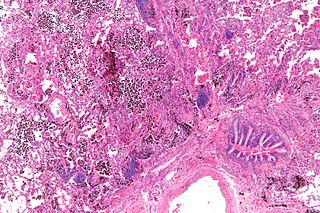
Pulmonary capillary hemangiomatosis (PCH) is a disease affecting the blood vessels of the lungs, where abnormal capillary proliferation and venous fibrous intimal thickening result in progressive increase in vascular resistance. It is a rare cause of pulmonary hypertension, and occurs predominantly in young adults. Together with pulmonary veno-occlusive disease, PCH comprises WHO Group I' causes for pulmonary hypertension. Indeed, there is some evidence to suggest that PCH and pulmonary veno-occlusive disease are different forms of a similar disease process.

Pulmonary veno-occlusive disease (PVOD) is a rare form of pulmonary hypertension caused by progressive blockage of the small veins in the lungs. The blockage leads to high blood pressures in the arteries of the lungs, which, in turn, leads to heart failure. The disease is progressive and fatal, with median survival of about 2 years from the time of diagnosis to death. The definitive therapy is lung transplantation.

Ventilation-perfusion coupling is the relationship between ventilation and perfusion processes, which take place in the respiratory and cardiovascular systems. Ventilation is the movement of gas during breathing, and perfusion is the process of pulmonary blood circulation, which delivers oxygen to body tissues. Anatomically, the lung structure, alveolar organization, and alveolar capillaries contribute to the physiological mechanism of ventilation and perfusion. Ventilation-perfusion coupling maintains a constant ratio near 0.8 on average, while the regional variation exists within the lungs due to gravity. When the ratio gets above or below 0.8, it is considered abnormal ventilation-perfusion coupling, also known as a ventilation-perfusion mismatch. Lung diseases, cardiac shunts, and smoking can cause a ventilation-perfusion mismatch that results in significant symptoms and diseases, which can be treated through treatments like bronchodilators and oxygen therapy.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Bishop, Naomi B.; Stankiewicz, Pawel; Steinhorn, Robin H. (15 July 2011). "Alveolar Capillary Dysplasia". American Journal of Respiratory and Critical Care Medicine. 184 (2): 172–179. doi:10.1164/rccm.201010-1697CI. PMC 3172887 . PMID 21471096.
- 1 2 3 Nogee, Lawrence M. (August 2017). "Interstitial lung disease in newborns". Seminars in Fetal and Neonatal Medicine. 22 (4): 227–233. doi:10.1016/j.siny.2017.03.003. PMC 5537026 . PMID 28363760.
- 1 2 Szafranski, Przemyslaw; Gambin, Tomasz; Dharmadhikari, Avinash V.; et al. (12 April 2016). "Pathogenetics of alveolar capillary dysplasia with misalignment of pulmonary veins". Human Genetics. 135 (5): 569–586. doi:10.1007/s00439-016-1655-9. PMC 5518754 . PMID 27071622.
- 1 2 Galambos, Csaba; Sims-Lucas, Sunder; Ali, Noorjahan; et al. (January 2015). "Intrapulmonary vascular shunt pathways in alveolar capillary dysplasia with misalignment of pulmonary veins". Thorax. 70 (1): 84–85. doi:10.1136/thoraxjnl-2014-205851. PMC 4405163 . PMID 25052575.
- 1 2 Janney, CG; Askin, FB; Kuhn C, 3rd (November 1981). "Congenital alveolar capillary dysplasia--an unusual cause of respiratory distress in the newborn". American Journal of Clinical Pathology. 76 (5): 722–7. doi:10.1093/ajcp/76.5.722. PMID 7293984.
- ↑ Kitayama Y, Kamata S, Okuyama H, Usui N, Sawai T, Kobayashi T, Fukui Y, Okada A (January 1997). "Nitric oxide inhalation therapy for an infant with persistent pulmonary hypertension caused by misalignment of pulmonary veins with alveolar capillary dysplasia". Journal of Pediatric Surgery. 32 (1): 99–100. doi:10.1016/s0022-3468(97)90105-6. PMID 9021581.
- ↑ MacMahon HE (July 1948). "Congenital alveolar dysplasia of the lungs". The American Journal of Pathology. 24 (4): 919–31. PMC 1942746 . PMID 18874417.
- ↑ MacMahon HE (July 1948). "Congenital alveolar dysplasia; a developmental anomaly involving pulmonary alveoli". Pediatrics. 2 (1): 43–57. doi:10.1542/peds.2.1.43. PMID 18874463. S2CID 245161989.
- ↑ Boggs S, Harris MC, Hoffman DJ, Goel R, McDonald-McGinn D, Langston C, Zackai E, Ruchelli E (January 1994). "Misalignment of pulmonary veins with alveolar capillary dysplasia: affected siblings and variable phenotypic expression". The Journal of Pediatrics. 124 (1): 125–8. doi:10.1016/S0022-3476(94)70267-5. PMID 8283361.