Eosinophils, sometimes called eosinophiles or, less commonly, acidophils, are a variety of white blood cells and one of the immune system components responsible for combating multicellular parasites and certain infections in vertebrates. Along with mast cells and basophils, they also control mechanisms associated with allergy and asthma. They are granulocytes that develop during hematopoiesis in the bone marrow before migrating into blood, after which they are terminally differentiated and do not multiply. They form about 2 to 3% of white blood cells in the body.

Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.

Enteritis is inflammation of the small intestine. It is most commonly caused by food or drink contaminated with pathogenic microbes, such as Serratia, but may have other causes such as NSAIDs, radiation therapy as well as autoimmune conditions like Crohn's disease and celiac disease. Symptoms include abdominal pain, cramping, diarrhea, dehydration, and fever. Related diseases of the gastrointestinal system involve inflammation of the stomach and large intestine.
Functional gastrointestinal disorders (FGID), also known as disorders of gut–brain interaction, include a number of separate idiopathic disorders which affect different parts of the gastrointestinal tract and involve visceral hypersensitivity and motility disturbances.
Eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as allergic granulomatosis, is an extremely rare autoimmune condition that causes inflammation of small and medium-sized blood vessels (vasculitis) in persons with a history of airway allergic hypersensitivity (atopy).
Food intolerance is a detrimental reaction, often delayed, to a food, beverage, food additive, or compound found in foods that produces symptoms in one or more body organs and systems, but generally refers to reactions other than food allergy. Food hypersensitivity is used to refer broadly to both food intolerances and food allergies.

Eosinophilic esophagitis (EoE) is an allergic inflammatory condition of the esophagus that involves eosinophils, a type of white blood cell. In healthy individuals, the esophagus is typically devoid of eosinophils. In EoE, eosinophils migrate to the esophagus in large numbers. When a trigger food is eaten, the eosinophils contribute to tissue damage and inflammation. Symptoms include swallowing difficulty, food impaction, vomiting, and heartburn.

Intestinal pseudo-obstruction (IPO) is a clinical syndrome caused by severe impairment in the ability of the intestines to push food through. It is characterized by the signs and symptoms of intestinal obstruction without any lesion in the intestinal lumen. Clinical features mimic those seen with mechanical intestinal obstructions and can include abdominal pain, nausea, abdominal distension, vomiting, dysphagia and constipation depending upon the part of the gastrointestinal tract involved.
Loeffler endocarditis is a form of heart disease characterized by a stiffened, poorly-functioning heart caused by infiltration of the heart by white blood cells known as eosinophils. Restrictive cardiomyopathy is a disease of the heart muscle which results in impaired diastolic filling of the heart ventricles, i.e. the large heart chambers which pump blood into the pulmonary or systemic circulation. Diastole is the part of the cardiac contraction-relaxation cycle in which the heart fills with venous blood after the emptying done during its previous systole.

Sucrose intolerance or genetic sucrase-isomaltase deficiency (GSID) is the condition in which sucrase-isomaltase, an enzyme needed for proper metabolism of sucrose (sugar) and starch, is not produced or the enzyme produced is either partially functional or non-functional in the small intestine. All GSID patients lack fully functional sucrase, while the isomaltase activity can vary from minimal functionality to almost normal activity. The presence of residual isomaltase activity may explain why some GSID patients are better able to tolerate starch in their diet than others with GSID.
Gluten-sensitive enteropathy–associated conditions are comorbidities or complications of gluten-related gastrointestinal distress. GSE has key symptoms typically restricted to the bowel and associated tissues; however, there are a wide variety of associated conditions. These include bowel disorders, eosinophilic gastroenteritis and increase with coeliac disease (CD) severity. With some early onset and a large percentage of late onset disease, other disorders appear prior to the coeliac diagnosis or allergic-like responses markedly increased in GSE. Many of these disorders persist on a strict gluten-free diet, and are thus independent of coeliac disease after triggering. For example, autoimmune thyroiditis is a common finding with GSE.

An esophageal food bolus obstruction is a medical emergency caused by the obstruction of the esophagus by an ingested foreign body.
An aeroallergen is any airborne substance, such as pollen or spores, which triggers an allergic reaction.

Eosinophilic bronchitis (EB) is a type of airway inflammation due to excessive mast cell recruitment and activation in the superficial airways as opposed to the smooth muscles of the airways as seen in asthma. It often results in a chronic cough. Lung function tests are usually normal. Inhaled corticosteroids are often an effective treatment.

Eosinophilic cystitis is a rare type of interstitial cystitis first reported in 1960 by Edwin Brown. Eosinophilic cystitis has been linked to a number of etiological factors, including allergies, bladder tumors, trauma to the bladder, parasitic infections, and chemotherapy drugs, though the exact cause of the condition is still unknown. The antigen-antibody response is most likely the cause of eosinophilic cystitis. This results in the generation of different immunoglobulins, which activate eosinophils and start the inflammatory process.
Non-celiac gluten sensitivity (NCGS) or gluten sensitivity is a controversial disorder which can cause both gastrointestinal and other problems.
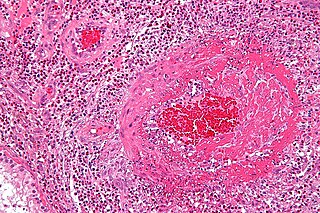
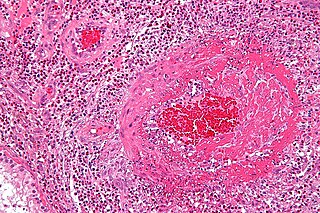
Eosinophilic myocarditis is inflammation in the heart muscle that is caused by the infiltration and destructive activity of a type of white blood cell, the eosinophil. Typically, the disorder is associated with hypereosinophilia, i.e. an eosinophil blood cell count greater than 1,500 per microliter. It is distinguished from non-eosinophilic myocarditis, which is heart inflammation caused by other types of white blood cells, i.e. lymphocytes and monocytes, as well as the respective descendants of these cells, NK cells and macrophages. This distinction is important because the eosinophil-based disorder is due to a particular set of underlying diseases and its preferred treatments differ from those for non-eosinophilic myocarditis.
Lymphocyte-variant hypereosinophilia is a rare disorder in which eosinophilia or hypereosinophilia is caused by an aberrant population of lymphocytes. These aberrant lymphocytes function abnormally by stimulating the proliferation and maturation of bone marrow eosinophil-precursor cells termed colony forming unit-eosinophils or CFU-Eos.
Familial eosinophilia is a rare congenital disorder characterized by the presence of sustained elevations in blood eosinophil levels that reach ranges diagnostic of eosinophilia or, far more commonly, hypereosinophilia. Although high eosinophil levels are associated with certain diseases and thought to contribute to the tissue destruction found in many other eosinophilia-related diseases, clinical manifestations and tissue destruction related to the eosinophilia in familial eosinophilia is uncommon: this genetic disease typically has a benign phenotype and course compared to other congenital and acquired eosinophilic diseases.

Lymphocytic esophagitis is a rare and poorly understood medical disorder involving inflammation in the esophagus. The disease is named from the primary inflammatory process, wherein lymphocytes are seen within the esophageal mucosa. Symptoms of the condition include difficulty swallowing, heartburn and food bolus obstruction. The condition was first described in 2006 by Rubio and colleagues. Initial reports questioned whether this was a true medical disorder, or whether the inflammation was secondary to another condition, such as gastroesophageal reflux disease.