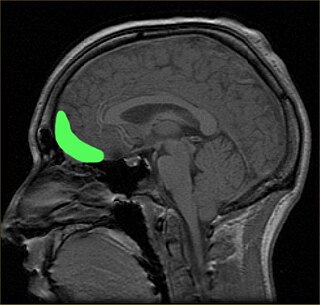
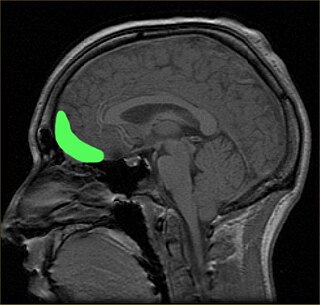
Bilateral cingulotomy is a form of psychosurgery, introduced in 1948 as an alternative to lobotomy. Today, it is mainly used in the treatment of depression and obsessive-compulsive disorder. In the early years of the twenty-first century, it was used in Russia to treat addiction. It is also used in the treatment of chronic pain. The objective of this procedure is the severing of the supracallosal fibres of the cingulum bundle, which pass through the anterior cingulate gyrus.
Phantom pain is a painful perception that an individual experiences relating to a limb or an organ that is not physically part of the body, either because it was removed or was never there in the first place.

A minimally conscious state or MCS is a disorder of consciousness distinct from persistent vegetative state and locked-in syndrome. Unlike persistent vegetative state, patients with MCS have partial preservation of conscious awareness. MCS is a relatively new category of disorders of consciousness. The natural history and longer term outcome of MCS have not yet been thoroughly studied. The prevalence of MCS was estimated to be 9 times of PVS cases, or between 112,000 and 280,000 in the US by year 2000.
The orbitofrontal cortex (OFC) is a prefrontal cortex region in the frontal lobes of the brain which is involved in the cognitive process of decision-making. In non-human primates it consists of the association cortex areas Brodmann area 11, 12 and 13; in humans it consists of Brodmann area 10, 11 and 47.
Emotional lateralization is the asymmetrical representation of emotional control and processing in the brain. There is evidence for the lateralization of other brain functions as well.
The causes of schizophrenia that underlie the development of schizophrenia, a psychiatric disorder, are complex and not clearly understood. A number of hypotheses including the dopamine hypothesis, and the glutamate hypothesis have been put forward in an attempt to explain the link between altered brain function and the symptoms and development of schizophrenia.

Meditation and its effect on brain activity and the central nervous system became a focus of collaborative research in neuroscience, psychology and neurobiology during the latter half of the 20th century. Research on meditation sought to define and characterize various practices. The effects of meditation on the brain can be broken up into two categories: state changes and trait changes, respectively alterations in brain activities during the act of meditating and changes that are the outcome of long-term practice.
Neuroimaging intelligence testing concerns the use of neuroimaging techniques to evaluate human intelligence. Neuroimaging technology has advanced such that scientists hope to use neuroimaging increasingly for investigations of brain function related to IQ.

Resting state fMRI is a method of functional magnetic resonance imaging (fMRI) that is used in brain mapping to evaluate regional interactions that occur in a resting or task-negative state, when an explicit task is not being performed. A number of resting-state brain networks have been identified, one of which is the default mode network. These brain networks are observed through changes in blood flow in the brain which creates what is referred to as a blood-oxygen-level dependent (BOLD) signal that can be measured using fMRI.

Hypofrontality is a state of decreased cerebral blood flow (CBF) in the prefrontal cortex of the brain. Hypofrontality is symptomatic of several neurological medical conditions, such as schizophrenia, attention deficit hyperactivity disorder (ADHD), bipolar disorder, and major depressive disorder. This condition was initially described by Ingvar and Franzén in 1974, through the use of xenon blood flow technique with 32 detectors to image the brains of patients with schizophrenia. This finding was confirmed in subsequent studies using the improved spatial resolution of positron emission tomography with the fluorodeoxyglucose (18F-FDG) tracer. Subsequent neuroimaging work has shown that the decreases in prefrontal CBF are localized to the medial, lateral, and orbital portions of the prefrontal cortex. Hypofrontality is thought to contribute to the negative symptoms of schizophrenia.

Katya Rubia is a professor of Cognitive Neuroscience at the MRC Social, Genetic and Developmental Psychiatry Centre and Department of Child and Adolescent Psychiatry, both part of the Institute of Psychiatry, King's College London.
Alcohol-related brain damage alters both the structure and function of the brain as a result of the direct neurotoxic effects of alcohol intoxication or acute alcohol withdrawal. Increased alcohol intake is associated with damage to brain regions including the frontal lobe, limbic system, and cerebellum, with widespread cerebral atrophy, or brain shrinkage caused by neuron degeneration. This damage can be seen on neuroimaging scans.
Chantal Stern is a neuroscientist who uses techniques including functional magnetic resonance imaging (fMRI) to study the brain mechanisms of memory function. She is the Director of the Brain, Behavior and Cognition program and a professor of Psychological and Brain Sciences at Boston University.After completing a degree at McGill University, she performed her doctoral research at Oxford University with Richard Passingham.
Neuromorality is an emerging field of neuroscience that studies the connection between morality and neuronal function. Scientists use fMRI and psychological assessment together to investigate the neural basis of moral cognition and behavior. Evidence shows that the central hub of morality is the prefrontal cortex guiding activity to other nodes of the neuromoral network. A spectrum of functional characteristics within this network to give rise to both altruistic and psychopathological behavior. Evidence from the investigation of neuromorality has applications in both clinical neuropsychiatry and forensic neuropsychiatry.
Vitaly Napadow is a Ukrainian-born American neuroscientist and acupuncturist. He is a full professor of Physical Medicine & Rehabilitation and Radiology at Harvard Medical School. He is also the Director of the Scott Schoen and Nancy Adams Discovery Center for Recovery from Chronic Pain at Spaulding Rehabilitation Hospital and Director of the Center for Integrative Pain NeuroImaging at the Martinos Center for Biomedical Imaging at Massachusetts General Hospital. He is a former president of the Society for Acupuncture Research. He has been a pain neuroimaging researcher for more than 20 years. Somatosensory, cognitive, and affective factors all influence the malleable experience of chronic pain, and Dr. Napadow’s Lab has applied human functional and structural neuroimaging to localize and suggest mechanisms by which different brain circuitries modulate pain perception. Dr. Napadow’s neuroimaging research also aims to better understand how non-pharmacological therapies, from acupuncture and transcutaneous neuromodulation to cognitive behavioral therapy and mindfulness meditation training, ameliorate aversive perceptual states such as pain. In fact, his early career was known for researching acupuncture and its effects on the brain. He has also researched the brain circuitry underlying nausea and itch. He is also known for developing a novel approach in applying measures of resting state brain connectivity as potential biomarkers for spontaneous clinical pain in chronic pain disorders such as fibromyalgia.
Meditation and pain is the study of the physiological mechanisms underlying meditation—specifically its neural components—that implicate it in the reduction of pain perception.

Bipolar disorder is an affective disorder characterized by periods of elevated and depressed mood. The cause and mechanism of bipolar disorder is not yet known, and the study of its biological origins is ongoing. Although no single gene causes the disorder, a number of genes are linked to increase risk of the disorder, and various gene environment interactions may play a role in predisposing individuals to developing bipolar disorder. Neuroimaging and postmortem studies have found abnormalities in a variety of brain regions, and most commonly implicated regions include the ventral prefrontal cortex and amygdala. Dysfunction in emotional circuits located in these regions have been hypothesized as a mechanism for bipolar disorder. A number of lines of evidence suggests abnormalities in neurotransmission, intracellular signalling, and cellular functioning as possibly playing a role in bipolar disorder.
Heather Clare Whalley is a Scottish scientist. She is a senior research fellow in neuroimaging at the Centre for Clinical Brain Sciences, University of Edinburgh, and is an affiliate member of the Centre for Genomic and Experimental Medicine at the University of Edinburgh. Her main focus of research is on the mechanisms underlying the development of major psychiatric disorders using the latest genomic and neuroimaging approaches.
Cassandra J. Lowe is a Canadian public health neuroscientist, specializing in understanding why some individuals have a hard time regulating junk food consumption. Lowe uses a multidimensional approach that combines repetitive transcranial magnetic stimulation (rTMS), neuroimaging and aerobic exercise to create causal models linking brain health to dietary decisions and behaviours. She was formally a BrainsCAN Postdoctoral Fellow within The Brain and Mind Institute and Department of Psychology at the University of Western Ontario, working with Dr. J. Bruce Morton and Dr. Lindsay Bodell. Since 2022, she has undertaken a position at the University of Exeter, in the United Kingdom as Lecturer in the School of Psychology.
Staci Ann Gruber is an Associate Professor of Psychiatry at Harvard Medical School and Director of the Cognitive and Clinical Neuroimaging Core (CCNC) and the Marijuana Investigation for Neuroscientific Discovery (MIND) Program. She is known for her work examining substance use and psychiatric conditions using advanced neuroimaging techniques and measures of cognitive performance.