The lungs are the main organs of the respiratory system in most terrestrial animals, including all tetrapod vertebrates and a small number of amphibious fish, pulmonate gastropods, and some arachnids. Their function is to conduct gas exchange by extracting oxygen from the air into the bloodstream via diffusion, and to release carbon dioxide from the bloodstream out into the atmosphere, a process also known as respiration. This article primarily concerns with the lungs of tetrapods, which are paired and located on either side of the heart, occupying most of the volume of the thoracic cavity, and are homologous to the swim bladders in ray-finned fish.

The respiratory tract is the subdivision of the respiratory system involved with the process of conducting air to the alveoli for the purposes of gas exchange in mammals. The respiratory tract is lined with respiratory epithelium as respiratory mucosa.

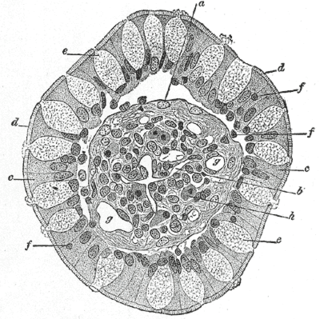
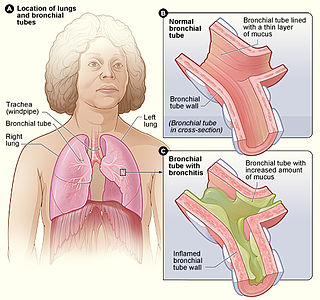
A bronchus is a passage or airway in the lower respiratory tract that conducts air into the lungs. The first or primary bronchi to branch from the trachea at the carina are the right main bronchus and the left main bronchus. These are the widest bronchi, and enter the right lung, and the left lung at each hilum. The main bronchi branch into narrower secondary bronchi or lobar bronchi, and these branch into narrower tertiary bronchi or segmental bronchi. Further divisions of the segmental bronchi are known as 4th order, 5th order, and 6th order segmental bronchi, or grouped together as subsegmental bronchi. The bronchi, when too narrow to be supported by cartilage, are known as bronchioles. No gas exchange takes place in the bronchi.

The bronchioles are the smaller branches of the bronchial airways in the lower respiratory tract. They include the terminal bronchioles, and finally the respiratory bronchioles that mark the start of the respiratory zone delivering air to the gas exchanging units of the alveoli. The bronchioles no longer contain the cartilage that is found in the bronchi, or glands in their submucosa.

Mucus is a slippery aqueous secretion produced by, and covering, mucous membranes. It is typically produced from cells found in mucous glands, although it may also originate from mixed glands, which contain both serous and mucous cells. It is a viscous colloid containing inorganic salts, antimicrobial enzymes, immunoglobulins, and glycoproteins such as lactoferrin and mucins, which are produced by goblet cells in the mucous membranes and submucosal glands. Mucus serves to protect epithelial cells in the linings of the respiratory, digestive, and urogenital systems, and structures in the visual and auditory systems from pathogenic fungi, bacteria and viruses. Most of the mucus in the body is produced in the gastrointestinal tract.
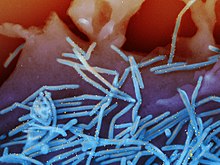
Club cells, also known as bronchiolar exocrine cells, are low columnar/cuboidal cells with short microvilli, found in the small airways (bronchioles) of the lungs. They were formerly known as Clara cells.
Goblet cells are simple columnar epithelial cells that secrete gel-forming mucins, like mucin 2 in the lower gastrointestinal tract, and mucin 5AC in the respiratory tract. The goblet cells mainly use the merocrine method of secretion, secreting vesicles into a duct, but may use apocrine methods, budding off their secretions, when under stress. The term goblet refers to the cell's goblet-like shape. The apical portion is shaped like a cup, as it is distended by abundant mucus laden granules; its basal portion lacks these granules and is shaped like a stem.
Acute severe asthma, also known as status asthmaticus, is an acute exacerbation of asthma that does not respond to standard treatments of bronchodilators (inhalers) and corticosteroids. Asthma is caused by multiple genes, some having protective effect, with each gene having its own tendency to be influenced by the environment although a genetic link leading to acute severe asthma is still unknown. Symptoms include chest tightness, rapidly progressive dyspnea, dry cough, use of accessory respiratory muscles, fast and/or labored breathing, and extreme wheezing. It is a life-threatening episode of airway obstruction and is considered a medical emergency. Complications include cardiac and/or respiratory arrest. The increasing prevalence of atopy and asthma remains unexplained but may be due to infection with respiratory viruses.

Respiratory epithelium, or airway epithelium, is a type of ciliated columnar epithelium found lining most of the respiratory tract as respiratory mucosa, where it serves to moisten and protect the airways. It is not present in the vocal cords of the larynx, or the oropharynx and laryngopharynx, where instead the epithelium is stratified squamous. It also functions as a barrier to potential pathogens and foreign particles, preventing infection and tissue injury by the secretion of mucus and the action of mucociliary clearance.

Erdosteine is a molecule with mucolytic activity. Structurally it is a thiol derivative characterized by the presence of two thiol groups. These two functional sulfhydryl groups contained in the molecule are released following first-pass metabolism with the conversion of erdosteine into its pharmacologically active metabolite Met-I.
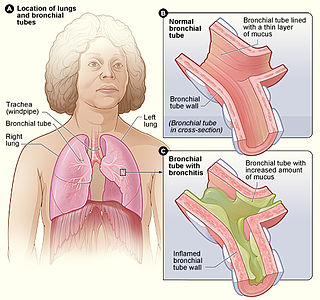
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.

Mucin-5AC(MUC-5AC) is a protein that is encoded by the MUC5AC gene in humans.

The intestinal epithelium is the single cell layer that forms the luminal surface (lining) of both the small and large intestine (colon) of the gastrointestinal tract. Composed of simple columnar epithelium its main functions are absorption, and secretion. Useful substances are absorbed into the body, and the entry of harmful substances is restricted. Secretions include mucins, and peptides.

Mucociliary clearance (MCC), mucociliary transport, or the mucociliary escalator describes the self-clearing mechanism of the airways in the respiratory system. It is one of the two protective processes for the lungs in removing inhaled particles including pathogens before they can reach the delicate tissue of the lungs. The other clearance mechanism is provided by the cough reflex. Mucociliary clearance has a major role in pulmonary hygiene.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.

Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms due to abnormalities of the airways and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.
The lung microbiota is the pulmonary microbial community consisting of a complex variety of microorganisms found in the lower respiratory tract particularly on the mucous layer and the epithelial surfaces. These microorganisms include bacteria, fungi, viruses and bacteriophages. The bacterial part of the microbiota has been more closely studied. It consists of a core of nine genera: Prevotella, Sphingomonas, Pseudomonas, Acinetobacter, Fusobacterium, Megasphaera, Veillonella, Staphylococcus, and Streptococcus. They are aerobes as well as anaerobes and aerotolerant bacteria. The microbial communities are highly variable in particular individuals and compose of about 140 distinct families. The bronchial tree for instance contains a mean of 2000 bacterial genomes per cm2 surface. The harmful or potentially harmful bacteria are also detected routinely in respiratory specimens. The most significant are Moraxella catarrhalis, Haemophilus influenzae, and Streptococcus pneumoniae. They are known to cause respiratory disorders under particular conditions namely if the human immune system is impaired. The mechanism by which they persist in the lower airways in healthy individuals is unknown.

The intestinal mucosal barrier, also referred to as intestinal barrier, refers to the property of the intestinal mucosa that ensures adequate containment of undesirable luminal contents within the intestine while preserving the ability to absorb nutrients. The separation it provides between the body and the gut prevents the uncontrolled translocation of luminal contents into the body proper. Its role in protecting the mucosal tissues and circulatory system from exposure to pro-inflammatory molecules, such as microorganisms, toxins, and antigens is vital for the maintenance of health and well-being. Intestinal mucosal barrier dysfunction has been implicated in numerous health conditions such as: food allergies, microbial infections, irritable bowel syndrome, inflammatory bowel disease, celiac disease, metabolic syndrome, non-alcoholic fatty liver disease, diabetes, and septic shock.
Donna Elizabeth Davies is a British biochemist and professor of respiratory cell and molecular biology at the University of Southampton. In 2003, Davies was the co-founder of Synairgen, an interferon-beta drug designed to treat patients with asthma and chronic obstructive pulmonary disease.