Related Research Articles
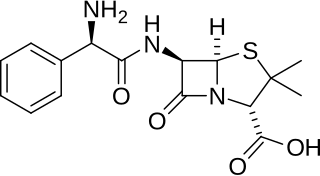
Ampicillin is an antibiotic belonging to the aminopenicillin class of the penicillin family. The drug is used to prevent and treat several bacterial infections, such as respiratory tract infections, urinary tract infections, meningitis, salmonellosis, and endocarditis. It may also be used to prevent group B streptococcal infection in newborns. It is used by mouth, by injection into a muscle, or intravenously.
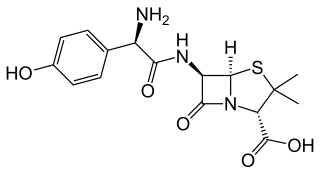
Amoxicillin is an antibiotic medication belonging to the aminopenicillin class of the penicillin family. The drug is used to treat bacterial infections such as middle ear infection, strep throat, pneumonia, skin infections, odontogenic infections, and urinary tract infections. It is taken orally, or less commonly by either intramuscular injection or by an IV bolus injection, which is a relatively quick intravenous injection lasting from a couple of seconds to a few minutes.
The HACEK organisms are a group of fastidious Gram-negative bacteria that are an unusual cause of infective endocarditis, which is an inflammation of the heart due to bacterial infection. HACEK is an abbreviation of the initials of the genera of this group of bacteria: Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, Kingella. The HACEK organisms are a normal part of the human microbiota, living in the oral-pharyngeal region.

Infective endocarditis is an infection of the inner surface of the heart (endocardium), usually the valves. Signs and symptoms may include fever, small areas of bleeding into the skin, heart murmur, feeling tired, and low red blood cell count. Complications may include backward blood flow in the heart, heart failure – the heart struggling to pump a sufficient amount of blood to meet the body's needs, abnormal electrical conduction in the heart, stroke, and kidney failure.

Cefazolin, also known as cefazoline and cephazolin, is a first-generation cephalosporin antibiotic used for the treatment of a number of bacterial infections. Specifically it is used to treat cellulitis, urinary tract infections, pneumonia, endocarditis, joint infection, and biliary tract infections. It is also used to prevent group B streptococcal disease around the time of delivery and before surgery. It is typically given by injection into a muscle or vein.

Amoxicillin/clavulanic acid, also known as co-amoxiclav or amox-clav, sold under the brand name Augmentin, among others, is an antibiotic medication used for the treatment of a number of bacterial infections. It is a combination consisting of amoxicillin, a β-lactam antibiotic, and potassium clavulanate, a β-lactamase inhibitor. It is specifically used for otitis media, streptococcal pharyngitis, pneumonia, cellulitis, urinary tract infections, and animal bites. It is taken by mouth or by injection into a vein.
Rat-bite fever (RBF) is an acute, febrile human illness caused by bacteria transmitted by rodents, in most cases, which is passed from rodent to human by the rodent's urine or mucous secretions. Alternative names for rat-bite fever include streptobacillary fever, streptobacillosis, spirillary fever, bogger, and epidemic arthritic erythema. It is a rare disease spread by infected rodents and caused by two specific types of bacteria:
- Streptobacillus moniliformis, the only reported bacteria that causes RBF in North America
- Spirillum minus, common in Asia. Most cases occur in Japan, but specific strains of the disease are present in the United States, Europe, Australia, and Africa.

Moraxella catarrhalis is a fastidious, nonmotile, Gram-negative, aerobic, oxidase-positive diplococcus that can cause infections of the respiratory system, middle ear, eye, central nervous system, and joints of humans. It causes the infection of the host cell by sticking to the host cell using trimeric autotransporter adhesins.

Imipenem/cilastatin, sold under the brand name Primaxin among others, is an antibiotic useful for the treatment of a number of bacterial infections. It is made from a combination of imipenem and cilastatin. Specifically it is used for pneumonia, sepsis, endocarditis, joint infections, intra-abdominal infections, and urinary tract infections. It is given by injection into a vein or muscle.
Antibiotic prophylaxis refers to, for humans, the prevention of infection complications using antimicrobial therapy. Antibiotic prophylaxis in domestic animal feed mixes has been employed in America since at least 1970.

Cefadroxil is a broad-spectrum antibiotic of the cephalosporin type, effective in Gram-positive and Gram-negative bacterial infections. It is a bactericidal antibiotic.

Sultamicillin, sold under the brand name Unasyn among others, is an oral form of the penicillin antibiotic combination ampicillin/sulbactam. It is used for the treatment of bacterial infections of the upper and lower respiratory tract, the kidneys and urinary tract, skin and soft tissues, among other organs. It contains esterified ampicillin and sulbactam.
Capnocytophaga is a genus of Gram-negative bacteria. Normally found in the oropharyngeal tract of mammals and are involved in the pathogenesis of some animal bite wounds and periodontal diseases.

Haverhill fever is a systemic illness caused by the bacterium Streptobacillus moniliformis, an organism common in rats and mice. If untreated, the illness can have a mortality rate of up to 13%. Among the two types of rat-bite fever, Haverhill fever caused by Streptobacillus moniliformis is most common in North America. The other type of infection caused by Spirillum minus is more common in Asia and is also known as Sodoku.
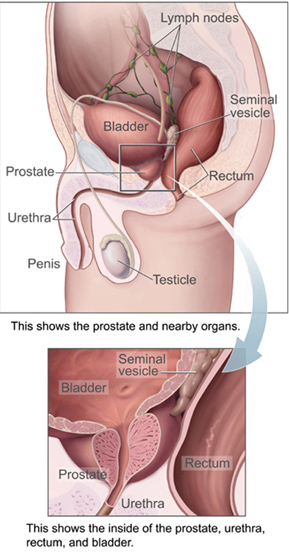
Chronic bacterial prostatitis (CBP) is a bacterial infection of the prostate gland and a form of prostatitis. It should be distinguished from other forms of prostatitis such as acute bacterial prostatitis (ABP) and chronic pelvic pain syndrome (CPPS).

Rothia dentocariosa is a species of Gram-positive, round- to rod-shaped bacteria that is part of the normal community of microbes residing in the mouth and respiratory tract.

Antibiotic misuse, sometimes called antibiotic abuse or antibiotic overuse, refers to the misuse or overuse of antibiotics, with potentially serious effects on health. It is a contributing factor to the development of antibiotic resistance, including the creation of multidrug-resistant bacteria, informally called "super bugs": relatively harmless bacteria can develop resistance to multiple antibiotics and cause life-threatening infections.

A periodontal abscess, is a localized collection of pus within the tissues of the periodontium. It is a type of dental abscess. A periodontal abscess occurs alongside a tooth, and is different from the more common periapical abscess, which represents the spread of infection from a dead tooth. To reflect this, sometimes the term "lateral (periodontal) abscess" is used. In contrast to a periapical abscess, periodontal abscesses are usually associated with a vital (living) tooth. Abscesses of the periodontium are acute bacterial infections classified primarily by location.
Dental antibiotic prophylaxis is the administration of antibiotics to a dental patient for prevention of harmful consequences of bacteremia, that may be caused by invasion of the oral flora into an injured gingival or peri-apical vessel during dental treatment.
References
- 1 2 Dar-Odeh, Najla Saeed; Abu-Hammad, Osama Abdalla; Al-Omiri, Mahmoud Khaled; Khraisat, Ameen Sameh; Shehabi, Asem Ata (2010). "Antibiotic prescribing practices by dentists: a review". Therapeutics and Clinical Risk Management. 6: 301–306. doi: 10.2147/tcrm.s9736 . ISSN 1176-6336. PMC 2909496 . PMID 20668712.
- 1 2 Riley, Philip; Glenny, Anne-Marie; Worthington, Helen V; Littlewood, Anne; Fernandez Mauleffinch, Luisa M; Clarkson, Jan E; McCabe, Martin G (2017-11-28). "Interventions for preventing oral mucositis in patients with cancer receiving treatment: cytokines and growth factors". Cochrane Database of Systematic Reviews. 2017 (11): CD011990. doi:10.1002/14651858.cd011990.pub2. ISSN 1465-1858. PMC 6486203 . PMID 29181845.
- ↑ Atlas, Ronald M. (1997). Principles of Microbiology (2 ed.). United States of America: Wm. C. Brown Publishers. pp. 1191. ISBN 9780815108894.
- 1 2 3 4 5 6 7 8 Newman, Michael G.; van Winkelhoff, Arie J. (2001). Antibiotic and Antimicrobial Use in Dental Practice (2 ed.). United States of America: Quintessence Publishing Co, Inc. p. 120.
- 1 2 3 4 5 Marsh, Professor Philip D.; Martin, Dr Michael V.; Lewis, Professor Michael A.O.; Williams, Dr David W. (2009). Oral Microbiology (5 ed.). Churchill Livingstone Elsevier. pp. 153. ISBN 9780443101441.
- ↑ "NHS urged to tackle antibiotic resistance | News and features | News | NICE". www.nice.org.uk. 18 November 2013. Retrieved 2016-11-25.
- 1 2 Rutherford, Samantha J.; Glenny, Anne-Marie; Roberts, Graham; Hooper, Lee; Worthington, Helen V. (2022-05-10). "Antibiotic prophylaxis for preventing bacterial endocarditis following dental procedures". The Cochrane Database of Systematic Reviews. 2022 (5): CD003813. doi:10.1002/14651858.CD003813.pub5. ISSN 1469-493X. PMC 9088886 . PMID 35536541.
- ↑ Yousefi, Yasamin. "Periodontal Abscess". National Library of Medicine.
- 1 2 3 4 Cope, Anwen; Francis, Nick; Wood, Fiona; Mann, Mala K; Chestnutt, Ivor G (2014-06-26). "Systemic antibiotics for symptomatic apical periodontitis and acute apical abscess in adults" (PDF). Cochrane Database of Systematic Reviews (6): CD010136. doi:10.1002/14651858.cd010136.pub2. PMID 24967571. S2CID 205203397.
- ↑ Cope, Anwen L.; Francis, Nick; Wood, Fiona; Chestnutt, Ivor G. (September 27, 2018). "Systemic antibiotics for symptomatic apical periodontitis and acute apical abscess in adults". The Cochrane Database of Systematic Reviews. 2018 (9): CD010136. doi:10.1002/14651858.CD010136.pub3. ISSN 1469-493X. PMC 6513530 . PMID 30259968.
- 1 2 3 4 5 6 Macfarlane, Samaranayake, T.Wallace, Lakshman P. Clinical oral microbiology. p. 218.
{{cite book}}: CS1 maint: multiple names: authors list (link) - 1 2 Rajendran, Arya; Sivapathasundharam, B. (2014). Elsevier Health Sciences APAC. Elsevier Health Sciences. p. 173. ISBN 978-81-312-3800-4.
- ↑ "Teeth whitening". bowriverdental.ca. 10 February 2014.
- ↑ Rajendran, Sivapathasundharam, Arya, B (2012). Shafer's Textbook of Oral Pathology (7th ed.). Elsevier India. ISBN 9788131230978.
{{cite book}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 5 Newman, Kornman, Michael, Kenneth. Antibiotic/Antimicrobial Use in Dental Practice. pp. 139, 142, 154, 164, 248.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ↑ Bhattacharya, Sanjib (2010). "The facts about penicillin allergy: a review". Journal of Advanced Pharmaceutical Technology & Research. 1 (1): 11–17. PMC 3255391 . PMID 22247826.
- 1 2 3 4 Rafael Poveda Roda, José Vicente Bagán, José María Sanchis Bielsa, Enrique Carbonell Pastor. "Antibiotic use in dental practice. A review" (PDF). Med Oral Patol Oral Cir Bucal. 12: 186–92.
{{cite journal}}: CS1 maint: multiple names: authors list (link)