Related Research Articles

Endocrinology is a branch of biology and medicine dealing with the endocrine system, its diseases, and its specific secretions known as hormones. It is also concerned with the integration of developmental events proliferation, growth, and differentiation, and the psychological or behavioral activities of metabolism, growth and development, tissue function, sleep, digestion, respiration, excretion, mood, stress, lactation, movement, reproduction, and sensory perception caused by hormones. Specializations include behavioral endocrinology and comparative endocrinology.

Addison's disease, also known as primary adrenal insufficiency, is a rare long-term endocrine disorder characterized by inadequate production of the steroid hormones cortisol and aldosterone by the two outer layers of the cells of the adrenal glands, causing adrenal insufficiency. Symptoms generally come on slowly and insidiously and may include abdominal pain and gastrointestinal abnormalities, weakness, and weight loss. Darkening of the skin in certain areas may also occur. Under certain circumstances, an adrenal crisis may occur with low blood pressure, vomiting, lower back pain, and loss of consciousness. Mood changes may also occur. Rapid onset of symptoms indicates acute adrenal failure, which is a clinical emergency. An adrenal crisis can be triggered by stress, such as from an injury, surgery, or infection.

Pernicious anemia is a disease where not enough red blood cells are produced due to a deficiency of vitamin B12. Those affected often have a gradual onset. The most common initial symptoms are feeling tired and weak. Other symptoms may include shortness of breath, feeling faint, a smooth red tongue, pale skin, chest pain, nausea and vomiting, loss of appetite, heartburn, numbness in the hands and feet, difficulty walking, memory loss, muscle weakness, poor reflexes, blurred vision, clumsiness, depression, and confusion. Without treatment, some of these problems may become permanent.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal glands—also referred to as the adrenal cortex—normally secrete glucocorticoids, mineralocorticoids, and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes to organ failure and shock. Adrenal crisis may occur if a person having adrenal insufficiency experiences stresses, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow.
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. Most cases are acquired ("secondary") due to extrinsic factors that affect the patient's immune system. Examples of these extrinsic factors include HIV infection and environmental factors, such as nutrition. Immunocompromisation may also be due to genetic diseases/flaws such as SCID.

Autoimmune polyendocrine syndromes (APSs), also called polyglandular autoimmune syndromes (PGASs) or polyendocrine autoimmune syndromes (PASs), are a heterogeneous group of rare diseases characterized by autoimmune activity against more than one endocrine organ, although non-endocrine organs can be affected. There are three types of APS, and there are a number of other diseases which involve endocrine autoimmunity.

Hashimoto's thyroiditis, also known as chronic lymphocytic thyroiditis, Hashimoto's disease, and autoimmune thyroiditis is an autoimmune disease in which the thyroid gland is gradually destroyed.

Gastritis is the inflammation of the lining of the stomach. It may occur as a short episode or may be of a long duration. There may be no symptoms but, when symptoms are present, the most common is upper abdominal pain. Other possible symptoms include nausea and vomiting, bloating, loss of appetite and heartburn. Complications may include stomach bleeding, stomach ulcers, and stomach tumors. When due to autoimmune problems, low red blood cells due to not enough vitamin B12 may occur, a condition known as pernicious anemia.
Achlorhydria and hypochlorhydria refer to states where the production of hydrochloric acid in gastric secretions of the stomach and other digestive organs is absent or low, respectively. It is associated with various other medical problems.

Atrophic gastritis is a process of chronic inflammation of the gastric mucosa of the stomach, leading to a loss of gastric glandular cells and their eventual replacement by intestinal and fibrous tissues. As a result, the stomach's secretion of essential substances such as hydrochloric acid, pepsin, and intrinsic factor is impaired, leading to digestive problems. The most common are pernicious anemia possibly leading to vitamin B12 deficiency; and malabsorption of iron, leading to iron deficiency anaemia. It can be caused by persistent infection with Helicobacter pylori, or can be autoimmune in origin. Those with autoimmune atrophic gastritis (Type A gastritis) are statistically more likely to develop gastric carcinoma, Hashimoto's thyroiditis, and achlorhydria.

Adrenocorticotropic hormone deficiency is a rare disorder characterized by secondary adrenal insufficiency with minimal or no cortisol production and normal pituitary hormone secretion apart from ACTH. ACTH deficiency may be congenital or acquired, and its symptoms are clinically similar to those of glucocorticoid deficiency. Symptoms consist of weight loss, diminished appetite, muscle weakness, nausea, vomiting, and hypotension. Low blood sugar and hyponatremia are possible; however, blood potassium levels typically remain normal because affected patients are deficient in glucocorticoids rather than mineralocorticoids because of their intact renin-angiotensin-aldosterone system. ACTH may be undetectable in blood tests, and cortisol is abnormally low. Glucocorticoid replacement therapy is required. With the exception of stressful situations, some patients with mild or nearly asymptomatic disease may not require glucocorticoid replacement therapy. As of 2008 about two hundred cases have been described in the literature.

Immunodysregulation polyendocrinopathy enteropathy X-linked syndrome is a rare autoimmune disease. It is one of the autoimmune polyendocrine syndromes. Most often, IPEX presents with autoimmune enteropathy, dermatitis (eczema), and autoimmune endocrinopathy, but other presentations exist.

The autoimmune regulator (AIRE) is a protein that in humans is encoded by the AIRE gene. It is a 13kbp gene on chromosome 21q22.3 that encodes 545 amino acids. AIRE is a transcription factor expressed in the medulla of the thymus. It is part of the mechanism which eliminates self-reactive T cells that would cause autoimmune disease. It exposes T cells to normal, healthy proteins from all parts of the body, and T cells that react to those proteins are destroyed.
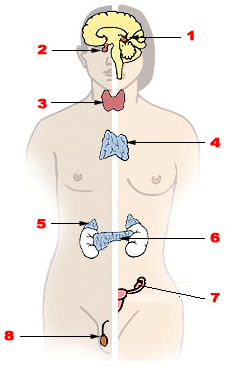
Endocrine diseases are disorders of the endocrine system. The branch of medicine associated with endocrine disorders is known as endocrinology.
Gluten-sensitive enteropathy–associated conditions are comorbidities or complications of gluten-related gastrointestinal distress. GSE has key symptoms typically restricted to the bowel and associated tissues; however, there are a wide variety of associated conditions. These include bowel disorders, eosinophilic gastroenteritis and increase with coeliac disease (CD) severity. With some early onset and a large percentage of late onset disease, other disorders appear prior to the coeliac diagnosis or allergic-like responses markedly increased in GSE. Many of these disorders persist on a strict gluten-free diet, and are thus independent of coeliac disease after triggering. For example, autoimmune thyroiditis is a common finding with GSE.
An immune disorder is a dysfunction of the immune system. These disorders can be characterized in several different ways:
Autoimmune polyendocrine syndrome type 2, a form of autoimmune polyendocrine syndrome also known as APS-II, or PAS II, is the most common form of the polyglandular failure syndromes. PAS II is defined as the association between autoimmune Addison's disease and either autoimmune thyroid disease, type 1 diabetes, or both. It is heterogeneous and has not been linked to one gene. Rather, individuals are at a higher risk when they carry a particular human leukocyte antigen. APS-II affects women to a greater degree than men.

Autoimmune polyendocrine syndrome type 1 (APS-1), is a subtype of autoimmune polyendocrine syndrome. It causes the dysfunction of multiple endocrine glands due to autoimmunity. It is a genetic disorder, inherited in autosomal recessive fashion due to a defect in the AIRE gene , which is located on chromosome 21 and normally confers immune tolerance.

Autoimmune enteropathy is a rare autoimmune disorder characterized by weight loss from malabsorption, severe and protracted diarrhea, and autoimmune damage to the intestinal mucosa. Autoimmune enteropathy typically occurs in infants and younger children however, adult cases have been reported in literature. Autoimmune enteropathy was first described by Walker-Smith et al. in 1982.
References
- ↑ "Monarch Initiative". Monarch Initiative. Retrieved January 27, 2024.
- ↑ Betterle, Corrado; Garelli, Silvia; Coco, Graziella; Burra, Patrizia (February 11, 2014). "A rare combination of type 3 autoimmune polyendocrine syndrome (APS-3) or multiple autoimmune syndrome (MAS-3)". Autoimmunity Highlights. 5 (1). Springer Science and Business Media LLC: 27–31. doi:10.1007/s13317-013-0055-6. ISSN 2038-0305. PMC 4389012 . PMID 26000153.
- ↑ Apolinario, Michael; Brussels, Aaron; Cook, Curtiss B.; Yang, Shaun (2022). "Autoimmune polyglandular syndrome type 3: A case report of an unusual presentation and literature review". Clinical Case Reports. 10 (2): e05391. doi:10.1002/ccr3.5391. ISSN 2050-0904. PMC 8815091 . PMID 35140971.
- 1 2 3 4 5 6 Quintos, Jb; Grover, Monica; Boney, Charlotte M; Salas, Max (2010). "Autoimmune polyglandular syndrome Type 3 and growth hormone deficiency". Pediatric Diabetes. 11 (6): 438–442. doi:10.1111/j.1399-5448.2009.00622.x. PMID 19968812. S2CID 8964242.
- ↑ Warncke, Katharina; Fröhlich-Reiterer, Elke E.; Thon, Angelika; Hofer, Sabine E.; Wiemann, Dagobert; Holl, Reinhard W. (June 14, 2010). "Polyendocrinopathy in Children, Adolescents, and Young Adults With Type 1 Diabetes". Diabetes Care. 33 (9). American Diabetes Association: 2010–2012. doi:10.2337/dc10-0404. ISSN 0149-5992. PMC 2928352 . PMID 20551013.
- ↑ Lahner, Edith; Centanni, Marco; Agnello, Giacoma; Gargano, Lucilla; Vannella, Lucy; Iannoni, Carlo; Delle Fave, Gianfranco; Annibale, Bruno (2008). "Occurrence and Risk Factors for Autoimmune Thyroid Disease in Patients with Atrophic Body Gastritis". The American Journal of Medicine. 121 (2). Elsevier BV: 136–141. doi:10.1016/j.amjmed.2007.09.025. ISSN 0002-9343. PMID 18261502.
- ↑ Frommer, Lara; Kahaly, George J (April 26, 2019). "Autoimmune Polyendocrinopathy". The Journal of Clinical Endocrinology & Metabolism. 104 (10). The Endocrine Society: 4769–4782. doi:10.1210/jc.2019-00602. ISSN 0021-972X. PMID 31127843.