Nasogastric intubation is a medical process involving the insertion of a plastic tube through the nose, down the esophagus, and down into the stomach. Orogastric intubation is a similar process involving the insertion of a plastic tube through the mouth. Abraham Louis Levin invented the NG tube. Nasogastric tube is also known as Ryle's tube in Commonwealth countries, after John Alfred Ryle.

Upper gastrointestinal bleeding is gastrointestinal bleeding (hemorrhage) in the upper gastrointestinal tract, commonly defined as bleeding arising from the esophagus, stomach, or duodenum. Blood may be observed in vomit or in altered form as black stool. Depending on the amount of the blood loss, symptoms may include shock.
Hematemesis is the vomiting of blood. It can be confused with hemoptysis or epistaxis (nosebleed), which are more common. The source is generally the upper gastrointestinal tract, typically above the suspensory muscle of duodenum. It may be caused by ulcers, tumors of the stomach or esophagus, varices, prolonged and vigorous retching, gastroenteritis, ingested blood, or certain drugs.

Misoprostol is a synthetic prostaglandin medication used to prevent and treat stomach and duodenal ulcers, induce labor, cause an abortion, and treat postpartum bleeding due to poor contraction of the uterus. It is taken by mouth when used to prevent gastric ulcers in people taking nonsteroidal anti-inflammatory drugs (NSAID). For abortions it is used by itself or in conjunction with mifepristone or methotrexate. By itself, effectiveness for abortion is between 66% and 90%. For labor induction or abortion, it is taken by mouth, dissolved in the mouth, or placed in the vagina. For postpartum bleeding it may also be used rectally.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Esophageal varices are extremely dilated sub-mucosal veins in the lower third of the esophagus. They are most often a consequence of portal hypertension, commonly due to cirrhosis. People with esophageal varices have a strong tendency to develop severe bleeding which left untreated can be fatal. Esophageal varices are typically diagnosed through an esophagogastroduodenoscopy.

Gastrointestinal bleeding, also called gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool. Small amounts of bleeding over a long time may cause iron-deficiency anemia resulting in feeling tired or heart-related chest pain. Other symptoms may include abdominal pain, shortness of breath, pale skin, or passing out. Sometimes in those with small amounts of bleeding no symptoms may be present.

Gastric varices are dilated submucosal veins in the lining of the stomach, which can be a life-threatening cause of bleeding in the upper gastrointestinal tract. They are most commonly found in patients with portal hypertension, or elevated pressure in the portal vein system, which may be a complication of cirrhosis. Gastric varices may also be found in patients with thrombosis of the splenic vein, into which the short gastric veins that drain the fundus of the stomach flow. The latter may be a complication of acute pancreatitis, pancreatic cancer, or other abdominal tumours, as well as hepatitis C. Gastric varices and associated bleeding are a potential complication of schistosomiasis resulting from portal hypertension.

Cervical effacement or cervical ripening refers to the thinning and shortening of the cervix. This process occurs during labor to prepare the cervix for dilation to allow the fetus to pass through the vagina. While this a normal, physiological process that occurs at the later end of pregnancy, it can also be induced through medications and procedures.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).

Uterine artery embolization is a procedure in which an interventional radiologist uses a catheter to deliver small particles that block the blood supply to the uterine body. The procedure is primarily done for the treatment of uterine fibroids and adenomyosis. Since uterine fibroids are the most common indication, it is also often referred to as uterine fibroid embolization. Compared to surgical treatment for fibroids such as a hysterectomy, in which a woman's uterus is removed, uterine artery embolization may be beneficial in women who wish to retain their uterus. Other reasons for uterine artery embolization are postpartum hemorrhage and uterine arteriovenous malformations.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.

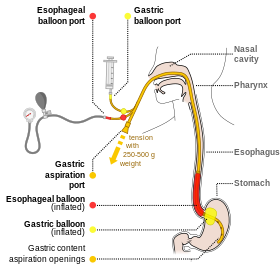
A Sengstaken–Blakemore tube is a medical device inserted through the nose or mouth and used occasionally in the management of upper gastrointestinal hemorrhage due to esophageal varices. The use of the tube was originally described in 1950, although similar approaches to bleeding varices were described by Westphal in 1930. With the advent of modern endoscopic techniques which can rapidly and definitively control variceal bleeding, Sengstaken–Blakemore tubes are rarely used at present.

Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood following childbirth. Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist. Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and an increased breathing rate. As more blood is lost, the patient may feel cold, blood pressure may drop, and they may become restless or unconscious. The condition can occur up to six weeks following delivery.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
The following outline is provided as an overview of and topical guide to obstetrics:
Round ligament pain (RLP) is pain associated with the round ligament of the uterus, usually during pregnancy. RLP is one of the most common discomforts of pregnancy and usually starts at the second trimester of gestation and continues until delivery. It usually resolves completely after delivery although cases of postpartum RLP have been reported. RLP also occurs in nonpregnant women.
The Bakri balloon is a medical device invented and designed by Dr. Younes Bakri in 1999.
Sayeba Akhter is a Bangladeshi physician who has dedicated her career to eliminating obstetric fistula. She is an executive member of the International Society of Obstetric Fistula Surgeons and has previously served as the president of the Obstetrics and Gynaecology Society of Bangladesh. She leads two charities, in Dhaka and Gaibandha, which focus on the education of underprivileged girls.
Uterine balloon tamponade (UBT) is a non-surgical method of treating refractory postpartum hemorrhage. Once postpartum hemorrhage has been identified and medical management given, UBT may be employed to tamponade uterine bleeding without the need to pursue operative intervention. Numerous studies have supported the efficacy of UBT as a means of managing refractory postpartum hemorrhage. The International Federation of Gynecology and Obstetrics (FIGO) and the World Health Organization (WHO) recommend UBT as second-line treatment for severe postpartum hemorrhage.