Karen Ann Quinlan was an American woman who became an important figure in the history of the right to die controversy in the United States.
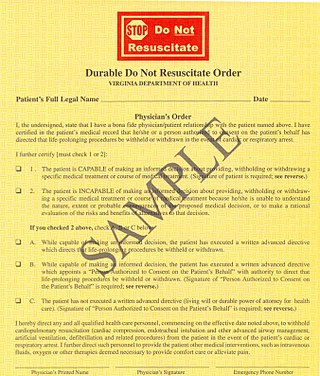
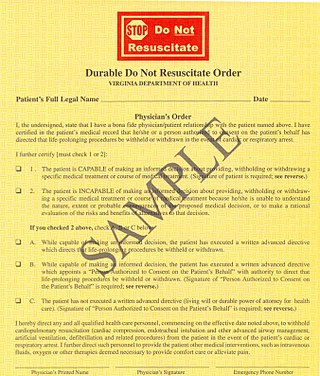
A do-not-resuscitate order (DNR), also known as Do Not Attempt Resuscitation (DNAR), Do Not Attempt Cardiopulmonary Resuscitation (DNACPR), no code or allow natural death, is a medical order, written or oral depending on country, indicating that a person should not receive cardiopulmonary resuscitation (CPR) if that person's heart stops beating. Sometimes these decisions and the relevant documents also encompass decisions around other critical or life-prolonging medical interventions. The legal status and processes surrounding DNR orders vary from country to country. Most commonly, the order is placed by a physician based on a combination of medical judgement and patient involvement.

Life support comprises the treatments and techniques performed in an emergency in order to support life after the failure of one or more vital organs. Healthcare providers and emergency medical technicians are generally certified to perform basic and advanced life support procedures; however, basic life support is sometimes provided at the scene of an emergency by family members or bystanders before emergency services arrive. In the case of cardiac injuries, cardiopulmonary resuscitation is initiated by bystanders or family members 25% of the time. Basic life support techniques, such as performing CPR on a victim of cardiac arrest, can double or even triple that patient's chance of survival. Other types of basic life support include relief from choking, staunching of bleeding by direct compression and elevation above the heart, first aid, and the use of an automated external defibrillator.
A persistent vegetative state (PVS) or post-coma unresponsiveness (PCU) is a disorder of consciousness in which patients with severe brain damage are in a state of partial arousal rather than true awareness. After four weeks in a vegetative state (VS), the patient is classified as being in a persistent vegetative state. This diagnosis is classified as a permanent vegetative state some months after a non-traumatic brain injury or one year after a traumatic injury. The term unresponsive wakefulness syndrome may be alternatively used, as "vegetative state" has some negative connotations among the public.
The right to die is a concept based on the opinion that human beings are entitled to end their life or undergo voluntary euthanasia. Possession of this right is often understood that a person with a terminal illness, incurable pain, or without the will to continue living, should be allowed to end their own life, use assisted suicide, or to decline life-prolonging treatment. The question of who, if anyone, may be empowered to make this decision is often the subject of debate.
Stephanie Keene, better known by the pseudonym Baby K, was an anencephalic baby who became the center of a major American court case and a debate among bioethicists.
Futile medical care is the continued provision of medical care or treatment to a patient when there is no reasonable hope of a cure or benefit.
The case of Sun Hudson concerned Wanda Hudson and her infant son, who was allowed to die via removal of his breathing tube, contrary to her wishes.
Cruzan v. Director, Missouri Department of Health, 497 U.S. 261 (1990), was a landmark decision of the Supreme Court of the United States involving a young adult incompetent. The first "right to die" case ever heard by the Court, Cruzan was argued on December 6, 1989, and decided on June 25, 1990. In a 5–4 decision, the Court affirmed the earlier ruling of the Supreme Court of Missouri and ruled in favor of the State of Missouri, finding it was acceptable to require "clear and convincing evidence" of a patient's wishes for removal of life support. A significant outcome of the case was the creation of advance health directives.

Bolam v Friern Hospital Management Committee [1957] 1 WLR 582 is an English tort law case that lays down the typical rule for assessing the appropriate standard of reasonable care in negligence cases involving skilled professionals such as doctors. This rule is known as the Bolam test, and states that if a doctor reaches the standard of a responsible body of medical opinion, they are not negligent. Bolam was rejected in the 2015 Supreme Court decision of Montgomery v Lanarkshire Health Board in matters of informed consent.
Anthony David Bland was a supporter of Liverpool F.C. injured in the Hillsborough disaster. He suffered severe brain damage that left him in a persistent vegetative state as a consequence of which the hospital, with the support of his parents, applied for a court order allowing him to "die with dignity". As a result, he became the first patient in English legal history to be allowed to die by the courts through the withdrawal of life-prolonging treatment including food and water.
Euthanasia is currently illegal in all 50 states of the United States. Assisted suicide is legal in 10 jurisdictions in the US: Washington, D.C. and the states of California, Colorado, Oregon, Vermont, New Mexico, Maine, New Jersey, Hawaii, and Washington. The status of assisted suicide is disputed in Montana, though currently authorized per the Montana Supreme Court's ruling in Baxter v. Montana that "nothing in Montana Supreme Court precedent or Montana statutes [indicates] that physician aid in dying is against public policy."
Eluana Englaro was an Italian woman from Lecco, who entered a persistent vegetative state on 18 January 1992, following a car accident, and subsequently became the focus of a court battle between supporters and opponents of euthanasia. Shortly after her accident, medical staff began feeding Englaro with a feeding tube, but her father "fought to have her feeding tube removed, saying it would be a dignified end to his daughter's life. He said that before the crash his daughter visited a friend who was in a coma and told him she didn't want the same thing to happen to her if she were ever in the same state." The authorities refused his request, but the decision was finally reversed in 2009, and she died after her nutrition was withheld after she had spent seventeen years in the persistent vegetative state.
Child euthanasia is a form of euthanasia that is applied to children who are gravely ill or have significant birth defects. In 2005, the Netherlands became the first country to decriminalize euthanasia for infants with hopeless prognosis and intractable pain. Nine years later, Belgium amended its 2002 Euthanasia Act to extend the rights of euthanasia to minors. Like euthanasia, there is world-wide public controversy and ethical debate over the moral, philosophical and religious issues of child euthanasia.
In re Quinlan was a landmark 1975 court case in the United States in which the parents of a woman who was kept alive by artificial means were allowed to order her removal from artificial ventilation.

Baxter v. Montana, is a Montana Supreme Court case, argued on September 2, 2009, and decided on December 31, 2009, that addressed the question of whether the state's constitution guaranteed terminally ill patients a right to lethal prescription medication from their physicians. The Montana Supreme Court sidestepped the question of if medical aid in dying is guaranteed under Montana State Constitution, but it instead ruled, on narrower grounds, that neither legal precedent nor the state's statute deem such assistance to be against public policy or illegal. Montana is one of ten states in which aid in dying is authorized. The others are California, Colorado, Hawaii, Maine, New Jersey, New Mexico, Oregon, Vermont, and Washington; it is authorized in the District of Columbia as well.
The Texas Advance Directives Act (1999), also known as the Texas Futile Care Law, describes certain provisions that are now Chapter 166 of the Texas Health & Safety Code. Controversy over these provisions mainly centers on Section 166.046, Subsection (e), which allows a health care facility to discontinue life-sustaining treatment ten days after giving written notice if the continuation of life-sustaining treatment is considered futile care by the treating medical team.
Since March 2018, passive euthanasia is legal in India under strict guidelines. Patients must consent through a living will, and must be either terminally ill or in a vegetative state.

Jahi McMath was a thirteen-year-old girl who was declared brain dead in California following surgery in 2013. This led to a bioethical debate engendered by her family's rejection of the medicolegal findings of death in the case, and their efforts to maintain her body using mechanical ventilation and other measures. Her parents considered these measures to constitute life support, while her doctors considered this to be futile treatment of a deceased person. In October 2014, the McMath family attorney made the unprecedented request that Jahi McMath's brain death declaration be overturned. The attorney later withdrew this request, saying he wanted time for the court-appointed medical expert and his own medical experts to confer. In March 2015, McMath's family filed a malpractice lawsuit against Children's Hospital Oakland and against the surgeon who performed McMath's surgery, indicating they were prepared to argue as part of the lawsuit that McMath is not dead, but profoundly disabled. The family lawyer stated that a preliminary second death certificate was issued on June 22, 2018, listing extensive bleeding relating to liver failure as the cause of death.

The Charlie Gard case was a best interests case in 2017 involving Charles Matthew William "Charlie" Gard, an infant boy from London, born with mitochondrial DNA depletion syndrome (MDDS), a rare genetic disorder that causes progressive brain damage and muscle failure. MDDS has no treatment and usually causes death in infancy. The case became controversial because the medical team and parents disagreed about whether experimental treatment was in the best interests of the child.