Hemolysis or haemolysis, also known by several other names, is the rupturing (lysis) of red blood cells (erythrocytes) and the release of their contents (cytoplasm) into surrounding fluid. Hemolysis may occur in vivo or in vitro.

Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired, life-threatening disease of the blood characterized by destruction of red blood cells by the complement system, a part of the body's innate immune system. This destructive process occurs due to deficiency of the red blood cell surface protein DAF, which normally inhibits such immune reactions. Since the complement cascade attacks the red blood cells within the blood vessels of the circulatory system, the red blood cell destruction (hemolysis) is considered an intravascular hemolytic anemia. There is ongoing research into other key features of the disease, such as the high incidence of venous blood clot formation. Research suggests that PNH thrombosis is caused by both the absence of GPI-anchored complement regulatory proteins on PNH platelets and the excessive consumption of nitric oxide (NO).

Hemolytic–uremic syndrome (HUS) is a group of blood disorders characterized by low red blood cells, acute kidney injury, and low platelets. Initial symptoms typically include bloody diarrhea, fever, vomiting, and weakness. Kidney problems and low platelets then occur as the diarrhea progresses. Children are more commonly affected, but most children recover without permanent damage to their health, although some children may have serious and sometimes life-threatening complications. Adults, especially the elderly, may present a more complicated presentation. Complications may include neurological problems and heart failure.

Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels or elsewhere in the human body (extravascular). This most commonly occurs within the spleen, but also can occur in the reticuloendothelial system or mechanically. Hemolytic anemia accounts for 5% of all existing anemias. It has numerous possible consequences, ranging from general symptoms to life-threatening systemic effects. The general classification of hemolytic anemia is either intrinsic or extrinsic. Treatment depends on the type and cause of the hemolytic anemia.

Budd–Chiari syndrome is a very rare condition, affecting one in a million adults. The condition is caused by occlusion of the hepatic veins that drain the liver.
Hypogammaglobulinemia is an immune system disorder in which not enough gamma globulins are produced in the blood. This results in a lower antibody count, which impairs the immune system, increasing risk of infection. Hypogammaglobulinemia may result from a variety of primary genetic immune system defects, such as common variable immunodeficiency, or it may be caused by secondary effects such as medication, blood cancer, or poor nutrition, or loss of gamma globulins in urine, as in nonselective glomerular proteinuria. Patients with hypogammaglobulinemia have reduced immune function; important considerations include avoiding use of live vaccines, and take precautionary measures when traveling to regions with endemic disease or poor sanitation such as receiving immunizations, taking antibiotics abroad, drinking only safe or boiled water, arranging appropriate medical cover in advance of travel, and ensuring continuation of any immunoglobulin infusions needed.
Paroxysmal cold hemoglobinuria (PCH) or Donath–Landsteiner hemolytic anemia (DLHA) is an autoimmune hemolytic anemia featured by complement-mediated intravascular hemolysis after cold exposure. It can present as an acute non-recurrent postinfectious event in children, or chronic relapsing episodes in adults with hematological malignancies or tertiary syphilis. Described by Julius Donath (1870–1950) and Karl Landsteiner (1868–1943) in 1904, PCH is one of the first clinical entities recognized as an autoimmune disorder.
Cold agglutinin disease (CAD) is a rare autoimmune disease characterized by the presence of high concentrations of circulating cold sensitive antibodies, usually IgM and autoantibodies that are also active at temperatures below 30 °C (86 °F), directed against red blood cells, causing them to agglutinate and undergo lysis. It is a form of autoimmune hemolytic anemia, specifically one in which antibodies bind red blood cells only at low body temperatures, typically 28–31 °C.

Protein losing enteropathy (PLE) is a syndrome in which blood proteins are lost excessively via the gastrointestinal (GI) tract. It may be caused by many different underlying diseases that damage the lining of the GI tract (mucosa) or cause blockage of its lymphatic drainage.
Eculizumab, sold under the brand name Soliris among others, is a recombinant humanized monoclonal antibody used to treat paroxysmal nocturnal hemoglobinuria, atypical hemolytic uremic syndrome, generalized myasthenia gravis, and neuromyelitis optica. In people with paroxysmal nocturnal hemoglobinuria, it reduces both the destruction of red blood cells and need for blood transfusion, but does not appear to affect the risk of death. Eculizumab was the first medication approved for each of its uses, and its approval was granted based on small trials. It is given by intravenous infusion. It is a humanized monoclonal antibody functioning as a terminal complement inhibitor. It binds to the complement C5 protein and inhibits activation of the complement system, a part of the body's immune system. This binding prevents the breakdown of red blood cells in the bloodstream in people with paroxysmal nocturnal hemoglobinuria and atypical hemolytic uremic syndrome.
Congenital hemolytic anemia (CHA) is a diverse group of rare hereditary conditions marked by decreased life expectancy and premature removal of erythrocytes from blood flow. Defects in erythrocyte membrane proteins and red cell enzyme metabolism, as well as changes at the level of erythrocyte precursors, lead to impaired bone marrow erythropoiesis. CAH is distinguished by variable anemia, chronic extravascular hemolysis, decreased erythrocyte life span, splenomegaly, jaundice, biliary lithiasis, and iron overload. Immune-mediated mechanisms may play a role in the pathogenesis of these uncommon diseases, despite the paucity of data regarding the immune system's involvement in CHAs.
Waldmann disease, also known as Primary Intestinal Lymphangiectasia (PIL), is a rare disease characterized by enlargement of the lymph vessels supplying the lamina propria of the small intestine. Although its prevalence is unknown, it being classified as a "rare disease" means that less than 200,000 of the population of the United States are affected by this condition and its subtypes and there have been approximately 50 reported cases of adult-onset PIL since 1961.
Atypical hemolytic uremic syndrome (aHUS), also known as complement-mediated hemolytic uremic syndrome, is an extremely rare, life-threatening, progressive disease that frequently has a genetic component. In most cases, it can be effectively controlled by interruption of the complement cascade. Particular monoclonal antibodies, discussed later in the article, have proven efficacy in many cases.

Autoimmune enteropathy is a rare autoimmune disorder characterized by weight loss from malabsorption, severe and protracted diarrhea, and autoimmune damage to the intestinal mucosa. Autoimmune enteropathy typically occurs in infants and younger children however, adult cases have been reported in literature. Autoimmune enteropathy was first described by Walker-Smith et al. in 1982.
Ravulizumab, sold under the brand name Ultomiris, is a humanized monoclonal antibody complement inhibitor medication designed for the treatment of paroxysmal nocturnal hemoglobinuria (PNH) and atypical hemolytic uremic syndrome. It is designed to bind to and prevent the activation of Complement component 5 (C5).
Pegcetacoplan, sold under the brand name Empaveli, among others, is a medication used to treat paroxysmal nocturnal hemoglobinuria and geographic atrophy of the retina. Pegcetacoplan is a complement inhibitor.

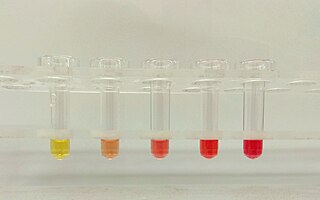
The sucrose lysis test is a diagnostic laboratory test used for diagnosing paroxysmal nocturnal hemoglobinuria (PNH), as well as for hypoplastic anemias and any hemolytic anemia with an unclear cause. The test works by using sucrose, which creates a low ionic strength environment that allows complement to bind to red blood cells. In individuals with PNH, some red blood cells are especially vulnerable to lysis caused by complement. The test may also produce suspicious results in other hematologic conditions, including megaloblastic anemia and autoimmune hemolytic anemia. False-negative results can occur when complement activity is absent in the serum. A simpler alternative called the sugar water test also involves mixing blood with sugar and observing for hemolysis, using the same principle as the sucrose lysis test.
Pozelimab, sold under the brand name Veopoz, is a recombinant monoclonal antibody used for the treatment of CD55-deficient protein-losing enteropathy, also known as CHAPLE disease. Pozelimab is a complement inhibitor. It is produced using recombinant DNA technology in Chinese hamster ovary cells.
Crovalimab, sold under the brand name Piasky, is a monoclonal antibody used for the treatment of people with paroxysmal nocturnal hemoglobinuria. It is a complement component 5 (C5) inhibitor.

Danicopan, sold under the brand name Voydeya, is a medication used for the treatment of paroxysmal nocturnal hemoglobinuria. It is a complement inhibitor which reversibly binds to factor D to prevent alternative pathway-mediated hemolysis and deposition of complement C3 proteins on red blood cells.