The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

Pancreatitis is a condition characterized by inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. There are two main types: acute pancreatitis, and chronic pancreatitis.

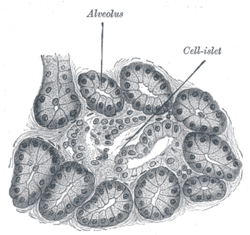
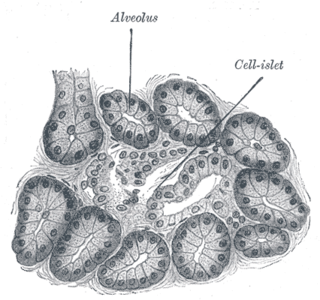
Exocrine glands are glands that secrete substances on to an epithelial surface by way of a duct. Examples of exocrine glands include sweat, salivary, mammary, ceruminous, lacrimal, sebaceous, prostate and mucous. Exocrine glands are one of two types of glands in the human body, the other being endocrine glands, which secrete their products directly into the bloodstream. The liver and pancreas are both exocrine and endocrine glands; they are exocrine glands because they secrete products—bile and pancreatic juice—into the gastrointestinal tract through a series of ducts, and endocrine because they secrete other substances directly into the bloodstream. Exocrine sweat glands are part of the integumentary system; they have eccrine and apocrine types.

Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. These cancerous cells have the ability to invade other parts of the body. A number of types of pancreatic cancer are known.

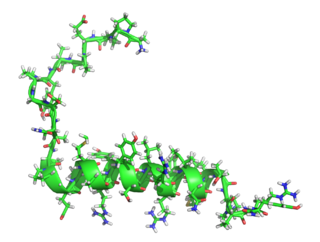
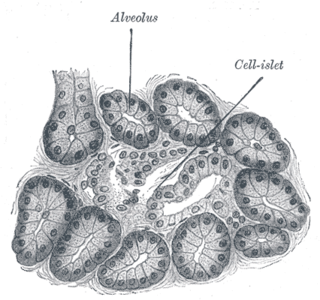
Pancreatic polypeptide cells, or formerly as gamma cells (γ-cells), or F cells, are cells in the pancreatic islets of the pancreas. Their main role is to help synthesize and regulate the release of pancreatic polypeptide (PP), after which they have been named. The pancreatic islets, where PP cells reside, was discovered in 1869 by a German pathological anatomist and scientist, Paul Langerhans. PP cells help to make up the pancreas but are smallest in proportion to the other cells previously stated. The proportions can vary based on which animals are being studied, but in humans, PP cells make up less than 2% of the pancreatic islet cell population.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes, in order of frequency, include: a gallstone impacted in the common bile duct beyond the point where the pancreatic duct joins it; heavy alcohol use; systemic disease; trauma; and, in minors, mumps. Acute pancreatitis may be a single event; it may be recurrent; or it may progress to chronic pancreatitis.

Chronic pancreatitis is a long-standing inflammation of the pancreas that alters the organ's normal structure and functions. It can present as episodes of acute inflammation in a previously injured pancreas, or as chronic damage with persistent pain or malabsorption. It is a disease process characterized by irreversible damage to the pancreas as distinct from reversible changes in acute pancreatitis.

Digestive enzymes are a group of enzymes that break down polymeric macromolecules into their smaller building blocks, in order to facilitate their absorption into the cells of the body. Digestive enzymes are found in the digestive tracts of animals and in the tracts of carnivorous plants, where they aid in the digestion of food, as well as inside cells, especially in their lysosomes, where they function to maintain cellular survival. Digestive enzymes of diverse specificities are found in the saliva secreted by the salivary glands, in the secretions of cells lining the stomach, in the pancreatic juice secreted by pancreatic exocrine cells, and in the secretions of cells lining the small and large intestines.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.
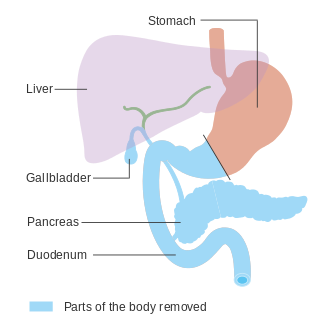
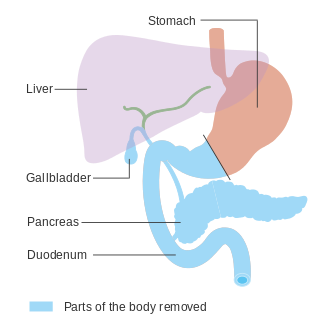
In medicine, a pancreatectomy is the surgical removal of all or part of the pancreas. Several types of pancreatectomy exist, including pancreaticoduodenectomy, distal pancreatectomy, segmental pancreatectomy, and total pancreatectomy. In recent years, the TP-IAT has also gained respectable traction within the medical community. These procedures are used in the management of several conditions involving the pancreas, such as benign pancreatic tumors, pancreatic cancer, and pancreatitis.

Exocrine pancreatic insufficiency (EPI) is the inability to properly digest food due to a lack or reduction of digestive enzymes made by the pancreas. EPI can occur in humans and is prevalent in many conditions such as cystic fibrosis, Shwachman–Diamond syndrome, different types of pancreatitis, multiple types of diabetes mellitus, advanced renal disease, older adults, celiac disease, IBS-D, IBD, HIV, alcohol-related liver disease, Sjogren syndrome, tobacco use, and use of somatostatin analogues.
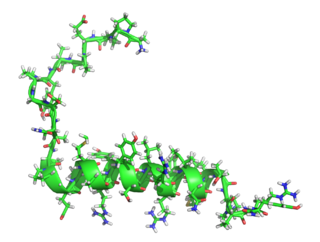
Pancreatic polypeptide (PP) is a polypeptide secreted by PP cells in the endocrine pancreas. It regulates pancreatic secretion activities, and also impacts liver glycogen storage and gastrointestinal secretion. Its secretion may be impacted by certain endocrine tumours.
Pancreatic diseases are diseases that affect the pancreas, an organ in most vertebrates and in humans and other mammals located in the abdomen. The pancreas plays a role in the digestive and endocrine system, producing enzymes which aid the digestion process and the hormone insulin, which regulates blood sugar levels. The most common pancreatic disease is pancreatitis, an inflammation of the pancreas which could come in acute or chronic form. Other pancreatic diseases include diabetes mellitus, exocrine pancreatic insufficiency, cystic fibrosis, pseudocysts, cysts, congenital malformations, tumors including pancreatic cancer, and hemosuccus pancreaticus.
Pancreatic elastase is a form of elastase that is produced in the acinar cells of the pancreas, initially produced as an inactive zymogen and later activated in the duodenum by trypsin. Elastases form a subfamily of serine proteases, characterized by a distinctive structure consisting of two beta barrel domains converging at the active site that hydrolyze amides and esters amongst many proteins in addition to elastin, a type of connective tissue that holds organs together. Pancreatic elastase 1 is a serine endopeptidase, a specific type of protease that has the amino acid serine at its active site. Although the recommended name is pancreatic elastase, it can also be referred to as elastase-1, pancreatopeptidase, PE, or serine elastase.
Diabetes mellitus is a disease in which the beta cells of the endocrine pancreas either stop producing insulin or can no longer produce it in enough quantity for the body's needs. The disease can affect humans as well as animals such as dogs.

Ductal cells refer to the epithelial cell lining of the pancreatic duct that deliver enzymes from the acinar cells to the duodenum. They have the essential function of producing bicarbonate-rich (HCO3-) secretion to neutralize stomach acidity. The hormone secretin stimulates ductal cells and is responsible for maintaining the duodenal pH and preventing duodenal injury from acidic chyme. Ductal cells mix their production with acinar cells to make up the pancreatic juice.

A pancreatic tumor is an abnormal growth in the pancreas. In adults, almost 90% are pancreatic cancer and a few are benign. Pancreatic tumors are rare in children.
Type 3c diabetes is diabetes that comes secondary to pancreatic diseases, involving the exocrine and digestive functions of the pancreas. It also occurs following surgical removal of the pancreas.

László Czakó is a Hungarian gastroenterologist, medical researcher, university professor and the deputy director of the First Department of Medicine, Albert Szent-Györgyi Health Center, Faculty of Medicine, University of Szeged. He is a notable and respected scientist both in Hungary and around the world in the field of gastroenterology.