Angiotensin-converting-enzyme inhibitors are a class of medication used primarily for the treatment of high blood pressure and heart failure. This class of medicine works by causing relaxation of blood vessels as well as a decrease in blood volume, which leads to lower blood pressure and decreased oxygen demand from the heart.

Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms itself. It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia. Hypertension is a major cause of premature death worldwide.

Renin, also known as an angiotensinogenase, is an aspartic protease protein and enzyme secreted by the kidneys that participates in the body's renin-angiotensin-aldosterone system (RAAS)—also known as the renin-angiotensin-aldosterone axis—that increases the volume of extracellular fluid and causes arterial vasoconstriction. Thus, it increases the body's mean arterial blood pressure.

The renin-angiotensin system (RAS), or renin-angiotensin-aldosterone system (RAAS), is a hormone system that regulates blood pressure, fluid, and electrolyte balance, and systemic vascular resistance.

Pulmonary edema, also known as pulmonary congestion, is excessive fluid accumulation in the tissue or air spaces of the lungs. This leads to impaired gas exchange, most often leading to shortness of breath (dyspnea) which can progress to hypoxemia and respiratory failure. Pulmonary edema has multiple causes and is traditionally classified as cardiogenic or noncardiogenic.
Essential hypertension is a form of hypertension without an identifiable physiologic cause. It is the most common type affecting 85% of those with high blood pressure. The remaining 15% is accounted for by various causes of secondary hypertension. Essential hypertension tends to be familial and is likely to be the consequence of an interaction between environmental and genetic factors. Hypertension can increase the risk of cerebral, cardiac, and renal events.

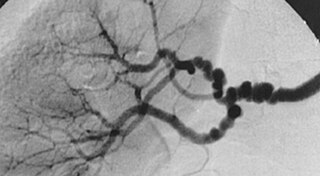
Renal artery stenosis (RAS) is the narrowing of one or both of the renal arteries, most often caused by atherosclerosis or fibromuscular dysplasia. This narrowing of the renal artery can impede blood flow to the target kidney, resulting in renovascular hypertension – a secondary type of high blood pressure. Possible complications of renal artery stenosis are chronic kidney disease and coronary artery disease.

The renal arteries are paired arteries that supply the kidneys with blood. Each is directed across the crus of the diaphragm, so as to form nearly a right angle.

Hypertensive kidney disease is a medical condition referring to damage to the kidney due to chronic high blood pressure. It manifests as hypertensive nephrosclerosis. It should be distinguished from renovascular hypertension, which is a form of secondary hypertension, and thus has opposite direction of causation.
Pseudohypertension, also known as pseudohypertension in the elderly, noncompressibility artery syndrome, and Osler's sign of pseudohypertension is a falsely elevated blood pressure reading obtained through sphygmomanometry due to calcification of blood vessels which cannot be compressed. There is normal blood pressure when it is measured from within the artery. This condition however is associated with significant cardiovascular disease risk.
Secondary hypertension is a type of hypertension which has a specific and identifiable underlying primary cause. It is much less common than essential hypertension, affecting only 5-10% of hypertensive patients. It has many different causes including obstructive sleep apnea, kidney disease, endocrine diseases, and tumors. The cause of secondary hypertension varies significantly with age. It also can be a side effect of many medications.

Renovascular hypertension is a condition in which high blood pressure is caused by the kidneys' hormonal response to narrowing of the arteries supplying the kidneys. When functioning properly this hormonal axis regulates blood pressure. Due to low local blood flow, the kidneys mistakenly increase blood pressure of the entire circulatory system. It is a form of secondary hypertension - a form of hypertension whose cause is identifiable.
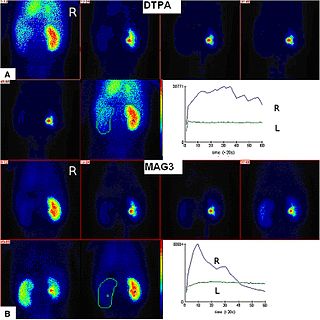
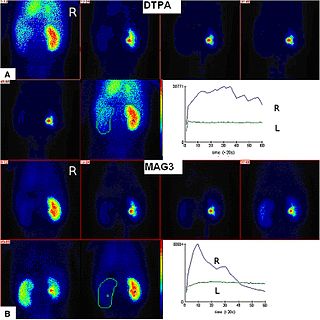
Radioisotope renography is a form of medical imaging of the kidneys that uses radiolabelling. A renogram, which may also be known as a MAG3 scan, allows a nuclear medicine physician or a radiologist to visualize the kidneys and learn more about how they are functioning. MAG3 is an acronym for mercapto acetyl tri glycine, a compound that is chelated with a radioactive element – technetium-99m.
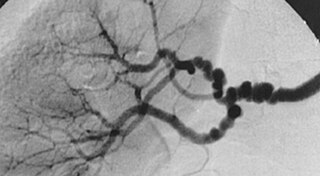
Fibromuscular dysplasia (FMD) is a non-atherosclerotic, non-inflammatory disease of the blood vessels that causes abnormal growth within the wall of an artery. FMD has been found in nearly every arterial bed in the body, although the most commonly affected are the renal and carotid arteries.
Pseudohyperaldosteronism is a medical condition which mimics the effects of elevated aldosterone (hyperaldosteronism) by presenting with high blood pressure, low blood potassium levels (hypokalemia), metabolic alkalosis, and low levels of plasma renin activity (PRA). However, unlike hyperaldosteronism, this conditions exhibits low or normal levels of aldosterone in the blood. Causes include genetic disorders, acquired conditions, metabolic disorders, and dietary imbalances including excessive consumption of licorice. Confirmatory diagnosis depends on the specific cause and may involve blood tests, urine tests, or genetic testing; however, all forms of this condition exhibit abnormally low concentrations of both plasma renin activity (PRA) and plasma aldosterone concentration (PAC) which differentiates this group of conditions from other forms of secondary hypertension. Treatment is tailored to the specific cause and focuses on symptom control, blood pressure management, and avoidance of triggers.
Hypertensive encephalopathy (HE) is general brain dysfunction due to significantly high blood pressure. Symptoms may include headache, vomiting, trouble with balance, and confusion. Onset is generally sudden. Complications can include seizures, posterior reversible encephalopathy syndrome, and bleeding in the back of the eye.

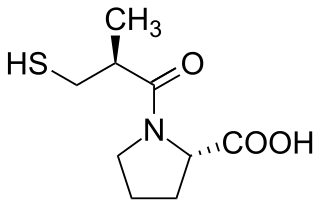
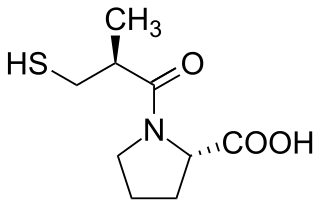
The captopril suppression test (CST) is a non-invasive medical test that measures plasma levels of aldosterone. Aldosterone production is suppressed by captopril through the renin–angiotensin–aldosterone system. CST results are used to assist in the diagnososis of primary aldosteronism.

Pathophysiology is a study which explains the function of the body as it relates to diseases and conditions. The pathophysiology of hypertension is an area which attempts to explain mechanistically the causes of hypertension, which is a chronic disease characterized by elevation of blood pressure. Hypertension can be classified by cause as either essential or secondary. About 90–95% of hypertension is essential hypertension. Some authorities define essential hypertension as that which has no known explanation, while others define its cause as being due to overconsumption of sodium and underconsumption of potassium. Secondary hypertension indicates that the hypertension is a result of a specific underlying condition with a well-known mechanism, such as chronic kidney disease, narrowing of the aorta or kidney arteries, or endocrine disorders such as excess aldosterone, cortisol, or catecholamines. Persistent hypertension is a major risk factor for hypertensive heart disease, coronary artery disease, stroke, aortic aneurysm, peripheral artery disease, and chronic kidney disease.

Orthostatic hypertension is a medical condition consisting of a sudden and abrupt increase in blood pressure (BP) when a person stands up. Orthostatic hypertension is diagnosed by a rise in systolic BP of 20 mmHg or more when standing. Orthostatic diastolic hypertension is a condition in which the diastolic BP raises to 98 mmHg or over in response to standing, but this definition currently lacks clear medical consensus, so is subject to change. Orthostatic hypertension involving the systolic BP is known as systolic orthostatic hypertension.
Kidney ischemia is a disease with a high morbidity and mortality rate. Blood vessels shrink and undergo apoptosis which results in poor blood flow in the kidneys. More complications happen when failure of the kidney functions result in toxicity in various parts of the body which may cause septic shock, hypovolemia, and a need for surgery. What causes kidney ischemia is not entirely known, but several pathophysiology relating to this disease have been elucidated. Possible causes of kidney ischemia include the activation of IL-17C and hypoxia due to surgery or transplant. Several signs and symptoms include injury to the microvascular endothelium, apoptosis of kidney cells due to overstress in the endoplasmic reticulum, dysfunctions of the mitochondria, autophagy, inflammation of the kidneys, and maladaptive repair.