Related Research Articles

The endocrine system is a messenger system comprising feedback loops of the hormones released by internal glands of an organism directly into the circulatory system, regulating distant target organs. In vertebrates, the hypothalamus is the neural control center for all endocrine systems. In humans, the major endocrine glands are the thyroid gland and the adrenal glands. The study of the endocrine system and its disorders is known as endocrinology.

In vertebrate anatomy, the pituitary gland, or hypophysis, is an endocrine gland, about the size of a pea and weighing 0.5 grams (0.018 oz) in humans. It is a protrusion off the bottom of the hypothalamus at the base of the brain. The hypophysis rests upon the hypophysial fossa of the sphenoid bone in the center of the middle cranial fossa and is surrounded by a small bony cavity covered by a dural fold. The anterior pituitary is a lobe of the gland that regulates several physiological processes including stress, growth, reproduction, and lactation. The intermediate lobe synthesizes and secretes melanocyte-stimulating hormone. The posterior pituitary is a lobe of the gland that is functionally connected to the hypothalamus by the median eminence via a small tube called the pituitary stalk.

Thyrotropin-releasing hormone (TRH) is a hypophysiotropic hormone produced by neurons in the hypothalamus that stimulates the release of thyroid-stimulating hormone (TSH) and prolactin from the anterior pituitary.
Luteinizing hormone is a hormone produced by gonadotropic cells in the anterior pituitary gland. The production of LH is regulated by gonadotropin-releasing hormone (GnRH) from the hypothalamus. In females, an acute rise of LH triggers ovulation and development of the corpus luteum. In males, where LH had also been called interstitial cell–stimulating hormone (ICSH), it stimulates Leydig cell production of testosterone. It acts synergistically with follicle-stimulating hormone (FSH).

Follicle-stimulating hormone (FSH) is a gonadotropin, a glycoprotein polypeptide hormone. FSH is synthesized and secreted by the gonadotropic cells of the anterior pituitary gland and regulates the development, growth, pubertal maturation, and reproductive processes of the body. FSH and luteinizing hormone (LH) work together in the reproductive system.
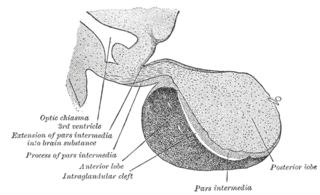
A major organ of the endocrine system, the anterior pituitary is the glandular, anterior lobe that together with the posterior lobe makes up the pituitary gland (hypophysis). The anterior pituitary regulates several physiological processes, including stress, growth, reproduction, and lactation. Proper functioning of the anterior pituitary and of the organs it regulates can often be ascertained via blood tests that measure hormone levels.

Hypopituitarism is the decreased (hypo) secretion of one or more of the eight hormones normally produced by the pituitary gland at the base of the brain. If there is decreased secretion of one specific pituitary hormone, the condition is known as selective hypopituitarism. If there is decreased secretion of most or all pituitary hormones, the term panhypopituitarism is used.
Neuroendocrine cells are cells that receive neuronal input and, as a consequence of this input, release message molecules (hormones) into the blood. In this way they bring about an integration between the nervous system and the endocrine system, a process known as neuroendocrine integration. An example of a neuroendocrine cell is a cell of the adrenal medulla, which releases adrenaline to the blood. The adrenal medullary cells are controlled by the sympathetic division of the autonomic nervous system. These cells are modified postganglionic neurons. Autonomic nerve fibers lead directly to them from the central nervous system. The adrenal medullary hormones are kept in vesicles much in the same way neurotransmitters are kept in neuronal vesicles. Hormonal effects can last up to ten times longer than those of neurotransmitters. Sympathetic nerve fiber impulses stimulate the release of adrenal medullary hormones. In this way the sympathetic division of the autonomic nervous system and the medullary secretions function together.
Releasing hormones and inhibiting hormones are hormones whose main purpose is to control the release of other hormones, either by stimulating or inhibiting their release. They are also called liberins and statins (respectively), or releasing factors and inhibiting factors. The principal examples are hypothalamic-pituitary hormones that can be classified from several viewpoints: they are hypothalamic hormones, they are hypophysiotropic hormones, and they are tropic hormones.

The hypothalamic–pituitary–gonadal axis refers to the hypothalamus, pituitary gland, and gonadal glands as if these individual endocrine glands were a single entity. Because these glands often act in concert, physiologists and endocrinologists find it convenient and descriptive to speak of them as a single system.

The hypophyseal portal system is a system of blood vessels in the microcirculation at the base of the brain, connecting the hypothalamus with the anterior pituitary. Its main function is to quickly transport and exchange hormones between the hypothalamus arcuate nucleus and anterior pituitary gland. The capillaries in the portal system are fenestrated which allows a rapid exchange between the hypothalamus and the pituitary. The main hormones transported by the system include gonadotropin-releasing hormone, corticotropin-releasing hormone, growth hormone–releasing hormone, and thyrotropin-releasing hormone.
Pituitary apoplexy is bleeding into or impaired blood supply of the pituitary gland. This usually occurs in the presence of a tumor of the pituitary, although in 80% of cases this has not been diagnosed previously. The most common initial symptom is a sudden headache, often associated with a rapidly worsening visual field defect or double vision caused by compression of nerves surrounding the gland. This is often followed by acute symptoms caused by lack of secretion of essential hormones, predominantly adrenal insufficiency.

The hypothalamic–pituitary–thyroid axis is part of the neuroendocrine system responsible for the regulation of metabolism and also responds to stress.
An insulin tolerance test (ITT) is a medical diagnostic procedure during which insulin is injected into a patient's vein, after which blood glucose is measured at regular intervals. This procedure is performed to assess pituitary function, adrenal function, insulin sensitivity, and sometimes for other purposes. An ITT is usually ordered and interpreted by endocrinologists.
The ACTH test is a medical test usually requested and interpreted by endocrinologists to assess the functioning of the adrenal glands' stress response by measuring the adrenal response to adrenocorticotropic hormone or another corticotropic agent such as tetracosactide or alsactide (Synchrodyn). ACTH is a hormone produced in the anterior pituitary gland that stimulates the adrenal glands to release cortisol, dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (DHEA-S), and aldosterone.
Hypothalamic–pituitary hormones are hormones that are produced by the hypothalamus and pituitary gland. Although the organs in which they are produced are relatively small, the effects of these hormones cascade throughout the body. They can be classified as a hypothalamic–pituitary axis of which the adrenal (HPA), gonadal (HPG), thyroid (HPT), somatotropic (HPS), and prolactin (HPP) axes are branches.
Hypothalamic disease is a disorder presenting primarily in the hypothalamus, which may be caused by damage resulting from malnutrition, including anorexia and bulimia eating disorders, genetic disorders, radiation, surgery, head trauma, lesion, tumour or other physical injury to the hypothalamus. The hypothalamus is the control center for several endocrine functions. Endocrine systems controlled by the hypothalamus are regulated by antidiuretic hormone (ADH), corticotropin-releasing hormone, gonadotropin-releasing hormone, growth hormone-releasing hormone, oxytocin, all of which are secreted by the hypothalamus. Damage to the hypothalamus may impact any of these hormones and the related endocrine systems. Many of these hypothalamic hormones act on the pituitary gland. Hypothalamic disease therefore affects the functioning of the pituitary and the target organs controlled by the pituitary, including the adrenal glands, ovaries and testes, and the thyroid gland.
Prior to the availability of sensitive TSH assays, thyrotropin releasing hormone or TRH stimulation tests were relied upon for confirming and assessing the degree of suppression in suspected hyperthyroidism. Typically, this stimulation test involves determining basal TSH levels and levels 15 to 30 minutes after an intravenous bolus of TRH. Normally, TSH would rise into the concentration range measurable with less sensitive TSH assays. Third generation TSH assays do not have this limitation and thus TRH stimulation is generally not required when third generation TSH assays are used to assess degree of suppression.
Hypogonadotropic hypogonadism (HH), is due to problems with either the hypothalamus or pituitary gland affecting the hypothalamic-pituitary-gonadal axis. Hypothalamic disorders result from a deficiency in the release of gonadotropic releasing hormone (GnRH), while pituitary gland disorders are due to a deficiency in the release of gonadotropins from the anterior pituitary. GnRH is the central regulator in reproductive function and sexual development via the HPG axis. GnRH is released by GnRH neurons, which are hypothalamic neuroendocrine cells, into the hypophyseal portal system acting on gonadotrophs in the anterior pituitary. The release of gonadotropins, LH and FSH, act on the gonads for the development and maintenance of proper adult reproductive physiology. LH acts on Leydig cells in the male testes and theca cells in the female. FSH acts on Sertoli cells in the male and follicular cells in the female. Combined this causes the secretion of gonadal sex steroids and the initiation of folliculogenesis and spermatogenesis. The production of sex steroids forms a negative feedback loop acting on both the anterior pituitary and hypothalamus causing a pulsatile secretion of GnRH. GnRH neurons lack sex steroid receptors and mediators such as kisspeptin stimulate GnRH neurons for pulsatile secretion of GnRH.
Pulsatile secretion is a biochemical phenomenon observed in a wide variety of cell and tissue types, in which chemical products are secreted in a regular temporal pattern. The most common cellular products observed to be released in this manner are intercellular signaling molecules such as hormones or neurotransmitters. Examples of hormones that are secreted pulsatilely include insulin, thyrotropin, TRH, gonadotropin-releasing hormone (GnRH) and growth hormone (GH). In the nervous system, pulsatility is observed in oscillatory activity from central pattern generators. In the heart, pacemakers are able to work and secrete in a pulsatile manner. A pulsatile secretion pattern is critical to the function of many hormones in order to maintain the delicate homeostatic balance necessary for essential life processes, such as development and reproduction. Variations of the concentration in a certain frequency can be critical to hormone function, as evidenced by the case of GnRH agonists, which cause functional inhibition of the receptor for GnRH due to profound downregulation in response to constant (tonic) stimulation. Pulsatility may function to sensitize target tissues to the hormone of interest and upregulate receptors, leading to improved responses. This heightened response may have served to improve the animal's fitness in its environment and promote its evolutionary retention.
References
- ↑ Yoshino A, Katayama Y, Watanabe T, et al. (June 2007). "Apoplexy accompanying pituitary adenoma as a complication of preoperative anterior pituitary function tests". Acta Neurochir (Wien). 149 (6): 557–65, discussion 565. doi:10.1007/s00701-007-1155-8. PMID 17468811. S2CID 24978106.
- ↑ Melmed, Shlomo (2002). The pituitary. Wiley-Blackwell. pp. 714–. ISBN 978-0-632-04357-6 . Retrieved 15 July 2011.
- ↑ Harsoulis P, Marshall JC, Kuku SF, Burke CW, London DR, Fraser TR (November 1973). "Combined test for assessment of anterior pituitary function". Br Med J. 4 (5888): 326–9. doi:10.1136/bmj.4.5888.326. PMC 1587416 . PMID 4202260.
- ↑ Greenwood FC, Landon J (May 1966). "Assessment of hypothalamic pituitary function in endocrine disease". J. Clin. Pathol. 19 (3): 284–92. doi:10.1136/jcp.19.3.284. PMC 473256 . PMID 4287115.