Related Research Articles

Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose below 70 mg/dL (3.9 mmol/L), symptoms associated with hypoglycemia, and resolution of symptoms when blood sugar returns to normal. Hypoglycemia may result in headache, tiredness, clumsiness, trouble talking, confusion, fast heart rate, sweating, shakiness, nervousness, hunger, loss of consciousness, seizures, or death. Symptoms typically come on quickly.
Insulin resistance (IR) is a pathological condition in which cells either fail to respond normally to the hormone insulin or downregulate insulin receptors in response to hyperinsulinemia.

The glucose tolerance test is a medical test in which glucose is given and blood samples taken afterward to determine how quickly it is cleared from the blood. The test is usually used to test for diabetes, insulin resistance, impaired beta cell function, and sometimes reactive hypoglycemia and acromegaly, or rarer disorders of carbohydrate metabolism. In the most commonly performed version of the test, an oral glucose tolerance test (OGTT), a standard dose of glucose is ingested by mouth and blood levels are checked two hours later. Many variations of the GTT have been devised over the years for various purposes, with different standard doses of glucose, different routes of administration, different intervals and durations of sampling, and various substances measured in addition to blood glucose.

Hyperglycemia is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a blood sugar level higher than 11.1 mmol/L (200 mg/dL), but symptoms may not start to become noticeable until even higher values such as 13.9–16.7 mmol/L (~250–300 mg/dL). A subject with a consistent range between ~5.6 and ~7 mmol/L is considered slightly hyperglycemic, and above 7 mmol/L is generally held to have diabetes. For diabetics, glucose levels that are considered to be too hyperglycemic can vary from person to person, mainly due to the person's renal threshold of glucose and overall glucose tolerance. On average, however, chronic levels above 10–12 mmol/L (180–216 mg/dL) can produce noticeable organ damage over time.

The hypothalamic–pituitary–adrenal axis is a complex set of direct influences and feedback interactions among three components: the hypothalamus, the pituitary gland, and the adrenal glands. These organs and their interactions constitute the HPA axis.

The blood sugar level, blood sugar concentration, blood glucose level, or glycemia, is the measure of glucose concentrated in the blood. The body tightly regulates blood glucose levels as a part of metabolic homeostasis.

Cortisol is a steroid hormone, in the glucocorticoid class of hormones. When used as a medication, it is known as hydrocortisone.

Addison's disease, also known as primary adrenal insufficiency, is a rare long-term endocrine disorder characterized by inadequate production of the steroid hormones cortisol and aldosterone by the two outer layers of the cells of the adrenal glands, causing adrenal insufficiency. Symptoms generally come on slowly and insidiously and may include abdominal pain and gastrointestinal abnormalities, weakness, and weight loss. Darkening of the skin in certain areas may also occur. Under certain circumstances, an adrenal crisis may occur with low blood pressure, vomiting, lower back pain, and loss of consciousness. Mood changes may also occur. Rapid onset of symptoms indicates acute adrenal failure, which is a clinical emergency. An adrenal crisis can be triggered by stress, such as from an injury, surgery, or infection.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal glands, also referred to as adrenal cortex normally secretes glucocorticoids, mineralocorticoids, and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes to organ failure and shock. Adrenal crisis may occur if a person having adrenal insufficiency experiences stresses, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow.

Hypopituitarism is the decreased (hypo) secretion of one or more of the eight hormones normally produced by the pituitary gland at the base of the brain. If there is decreased secretion of one specific pituitary hormone, the condition is known as selective hypopituitarism. If there is decreased secretion of most or all pituitary hormones, the term panhypopituitarism is used.
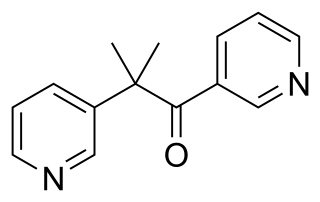
Metyrapone, sold under the brand name Metopirone, is a medication which is used in the diagnosis of adrenal insufficiency and occasionally in the treatment of Cushing's syndrome (hypercortisolism). It is part of the steroidogenesis inhibitor class of drugs.
Ketotic hypoglycemia is a medical term used in two ways: (1) broadly, to refer to any circumstance in which low blood glucose is accompanied by ketosis, and (2) also nutritional ketosis. It remains one of the more common causes of hypoglycemia in the age range.

Reactive hypoglycemia, postprandial hypoglycemia, or sugar crash is a term describing recurrent episodes of symptomatic hypoglycemia occurring within four hours after a high carbohydrate meal in people with and without diabetes. The term is not necessarily a diagnosis since it requires an evaluation to determine the cause of the hypoglycemia.
Chronic Somogyi rebound is a contested explanation of phenomena of elevated blood sugars experienced by diabetics in the morning. Also called the Somogyi effect and posthypoglycemic hyperglycemia, it is a rebounding high blood sugar that is a response to low blood sugar. When managing the blood glucose level with insulin injections, this effect is counter-intuitive to people who experience high blood sugar in the morning as a result of an overabundance of insulin at night.
A combined rapid anterior pituitary evaluation panel or triple bolus test or a dynamic pituitary function test is a medical diagnostic procedure used to assess a patient's pituitary function. A triple bolus test is usually ordered and interpreted by endocrinologists.
The ACTH test is a medical test usually requested and interpreted by endocrinologists to assess the functioning of the adrenal glands' stress response by measuring the adrenal response to adrenocorticotropic hormone or another corticotropic agent such as tetracosactide or alsactide (Synchrodyn). ACTH is a hormone produced in the anterior pituitary gland that stimulates the adrenal glands to release cortisol, dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (DHEA-S), and aldosterone.
Autoimmune hypophysitis is defined as inflammation of the pituitary gland due to autoimmunity.

Adrenal crisis is a potentially life-threatening medical condition requiring immediate emergency treatment. It is a constellation of symptoms that indicate severe adrenal insufficiency. This may be the result of either previously undiagnosed or untreated Addison's disease, a disease process suddenly affecting adrenal function, suddenly stopping intake of glucocorticoids or an intercurrent problem in someone known to have Addison's disease, congenital adrenal hyperplasia (CAH), or other form of primary adrenal insufficiency.
Critical illness–related corticosteroid insufficiency is a form of adrenal insufficiency in critically ill patients who have blood corticosteroid levels which are inadequate for the severe stress response they experience. Combined with decreased glucocorticoid receptor sensitivity and tissue response to corticosteroids, this adrenal insufficiency constitutes a negative prognostic factor for intensive care patients.
Hypoadrenocorticism in dogs, or, as it is known in people, Addison's disease, is an endocrine system disorder that occurs when the adrenal glands fail to produce enough hormones for normal function. The adrenal glands secrete glucocorticoids such as cortisol and mineralocorticoids such as aldosterone; when proper amounts of these are not produced, the metabolic and electrolyte balance is upset. Mineralocorticoids control the amount of potassium, sodium, and water in the body. Hypoadrenocorticism is fatal if left untreated.
References
- 1 2 Okita K, Iwahashi H, Kozawa J, Okauchi Y, Funahashi T, Imagawa A, Shimomura I (May 4, 2014). "Usefulness of the insulin tolerance test in patients with type 2 diabetes receiving insulin therapy". J Diabetes Investig. 5 (3): 305–312. doi:10.1111/jdi.12143. PMC 4020335 . PMID 24843779.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ "Insulin Tolerance Test (ITT)". Melior Discovery. Retrieved 1 October 2019.
- ↑ Greenwood FC, Landon J, Stamp TC (1965). "The plasma sugar, free fatty acid, cortisol, and growth hormone response to insulin. I. In control subjects". J Clin Invest. 45 (4): 429–. doi:10.1172/JCI105357. PMC 292717 . PMID 5937021.
- ↑ Plumpton FS, Besser GM (1969). "The adrenocortical response to surgery and insulin-induced hypoglycaemia in corticosteroid-treated and normal subjects". Br J Surg. 56 (3): 216–219. doi:10.1002/bjs.1800560315. PMID 5776687. S2CID 29500731.