Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose below 70 mg/dL (3.9 mmol/L), symptoms associated with hypoglycemia, and resolution of symptoms when blood sugar returns to normal. Hypoglycemia may result in headache, tiredness, clumsiness, trouble talking, confusion, fast heart rate, sweating, shakiness, nervousness, hunger, loss of consciousness, seizures, or death. Symptoms typically come on quickly.
The following is a glossary of diabetes which explains terms connected with diabetes.

Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of diabetes mellitus. Signs and symptoms may include vomiting, abdominal pain, deep gasping breathing, increased urination, weakness, confusion and occasionally loss of consciousness. A person's breath may develop a specific "fruity" smell. The onset of symptoms is usually rapid. People without a previous diagnosis of diabetes may develop DKA as the first obvious symptom.

Hyperglycemia or Hyperglycaemia is a condition in which an excessive amount of glucose (glucotoxicity) circulates in the blood plasma. This is generally a blood sugar level higher than 11.1 mmol/L (200 mg/dL), but symptoms may not start to become noticeable until even higher values such as 13.9–16.7 mmol/L (~250–300 mg/dL). A subject with a consistent fasting blood glucose range between ~5.6 and ~7 mmol/L is considered slightly hyperglycemic, and above 7 mmol/L is generally held to have diabetes. For diabetics, glucose levels that are considered to be too hyperglycemic can vary from person to person, mainly due to the person's renal threshold of glucose and overall glucose tolerance. On average, however, chronic levels above 10–12 mmol/L (180–216 mg/dL) can produce noticeable organ damage over time.
Ketoacidosis is a metabolic state caused by uncontrolled production of ketone bodies that cause a metabolic acidosis. While ketosis refers to any elevation of blood ketones, ketoacidosis is a specific pathologic condition that results in changes in blood pH and requires medical attention. The most common cause of ketoacidosis is diabetic ketoacidosis but can also be caused by alcohol, medications, toxins, and rarely, starvation.

Alcoholic ketoacidosis (AKA) is a specific group of symptoms and metabolic state related to alcohol use. Symptoms often include abdominal pain, vomiting, agitation, a fast respiratory rate, and a specific "fruity" smell. Consciousness is generally normal. Complications may include sudden death.
Hyperinsulinemic hypoglycemia describes the condition and effects of low blood glucose caused by excessive insulin. Hypoglycemia due to excess insulin is the most common type of serious hypoglycemia. It can be due to endogenous or injected insulin.
Neuroglycopenia is a shortage of glucose (glycopenia) in the brain, usually due to hypoglycemia. Glycopenia affects the function of neurons, and alters brain function and behavior. Prolonged or recurrent neuroglycopenia can result in loss of consciousness, damage to the brain, and eventual death.
Feline diabetes mellitus is a chronic disease in cats whereby either insufficient insulin response or insulin resistance leads to persistently high blood glucose concentrations. Diabetes affects up to 1 in 230 cats, and may be becoming increasingly common. Diabetes is less common in cats than in dogs. The condition is treatable, and if treated properly the cat can experience a normal life expectancy. In cats with type 2 diabetes, prompt effective treatment may lead to diabetic remission, in which the cat no longer needs injected insulin. Untreated, the condition leads to increasingly weak legs in cats and eventually to malnutrition, ketoacidosis and/or dehydration, and death.

Diabetic hypoglycemia is a low blood glucose level occurring in a person with diabetes mellitus. It is one of the most common types of hypoglycemia seen in emergency departments and hospitals. According to the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP), and based on a sample examined between 2004 and 2005, an estimated 55,819 cases involved insulin, and severe hypoglycemia is likely the single most common event.

Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that originates when cells that make insulin are destroyed by the immune system. Insulin is a hormone required for the cells to use blood sugar for energy and it helps regulate glucose levels in the bloodstream. It results in high blood sugar levels in the body prior to treatment. The common symptoms of this elevated blood sugar are frequent urination, increased thirst, increased hunger, weight loss, and other serious complications. Additional symptoms may include blurry vision, tiredness, and slow wound healing. Symptoms typically develop over a short period of time, often a matter of weeks if not months.
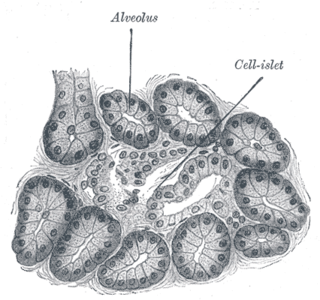
The term diabetes includes several different metabolic disorders that all, if left untreated, result in abnormally high concentrations of a sugar called glucose in the blood. Diabetes mellitus type 1 results when the pancreas no longer produces significant amounts of the hormone insulin, usually owing to the autoimmune destruction of the insulin-producing beta cells of the pancreas. Diabetes mellitus type 2, in contrast, is now thought to result from autoimmune attacks on the pancreas and/or insulin resistance. The pancreas of a person with type 2 diabetes may be producing normal or even abnormally large amounts of insulin. Other forms of diabetes mellitus, such as the various forms of maturity-onset diabetes of the young, may represent some combination of insufficient insulin production and insulin resistance. Some degree of insulin resistance may also be present in a person with type 1 diabetes.
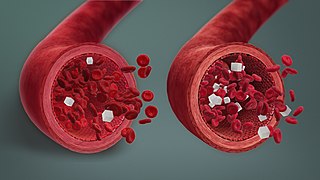
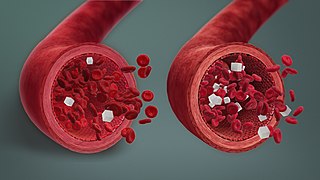
Hyperosmolar hyperglycemic state (HHS), also known as hyperosmolar non-ketotic state (HONK), is a complication of diabetes mellitus in which high blood sugar results in high osmolarity without significant ketoacidosis. Symptoms include signs of dehydration, weakness, leg cramps, vision problems, and an altered level of consciousness. Onset is typically over days to weeks. Complications may include seizures, disseminated intravascular coagulopathy, mesenteric artery occlusion, or rhabdomyolysis.
An insulin tolerance test (ITT) is a medical diagnostic procedure during which insulin is injected into a patient's vein, after which blood glucose is measured at regular intervals. This procedure is performed to assess pituitary function, adrenal function, insulin sensitivity, and sometimes for other purposes. An ITT is usually ordered and interpreted by an endocrinologist.
Chronic Somogyi rebound is a contested explanation of phenomena of elevated blood sugars experienced by diabetics in the morning. Also called the Somogyi effect and posthypoglycemic hyperglycemia, it is a rebounding high blood sugar that is a response to low blood sugar. When managing the blood glucose level with insulin injections, this effect is counter-intuitive to people who experience high blood sugar in the morning as a result of an overabundance of insulin at night.
Hyperosmolar syndrome or diabetic hyperosmolar syndrome is a medical emergency caused by a very high blood glucose level.
Complications of diabetes are secondary diseases that are a result of elevated blood glucose levels that occur in diabetic patients. These complications can be divided into two types: acute and chronic. Acute complications are complications that develop rapidly and can be exemplified as diabetic ketoacidosis (DKA), hyperglycemic hyperosmolar state (HHS), lactic acidosis (LA), and hypoglycemia. Chronic complications develop over time and are generally classified in two categories: microvascular and macrovascular. Microvascular complications include neuropathy, nephropathy, and retinopathy; while cardiovascular disease, stroke, and peripheral vascular disease are included in the macrovascular complications.
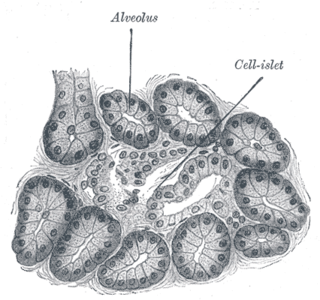
Diabetes mellitus is a disease in which the beta cells of the endocrine pancreas either stop producing insulin or can no longer produce it in enough quantity for the body's needs. The disease can affect humans as well as animals such as dogs.
Dysglycemia is a general definition for any abnormalities in blood glucose levels. They include hyperglycemia, hypoglycemia, impaired glucose tolerance test, impaired fasting glucose, among others.
Ketosis-prone diabetes (KPD) is an intermediate form of diabetes that has some characteristics of type 1 and some of type 2 diabetes. Type 1 diabetes involves autoimmune destruction of pancreatic beta cells which create insulin. This occurs earlier in a person's life, leading to patients being insulin dependent, and the lack of natural insulin makes patients prone to a condition called diabetic ketoacidosis (DKA). Type 2 diabetes is different in that it is usually caused by insulin resistance in the body in older patients leading to beta cell burnout over time, and is not prone to DKA. KPD is a condition that involves DKA like type 1, but occurs later in life and can regain beta cell function like type 2 diabetes. However, it is distinct from latent autoimmune diabetes of adults (LADA), a form of type 1 sometimes referred to as type 1.5 that does not occur with DKA. There are also distinctions to be made between KPD and LADA as patients who exhibit KPD symptoms can regain beta cell function similar to type 2 diabetics whereas LADA will not exhibit this reclamation of beta cell function.