Hypnotic, or soporific drugs, commonly known as sleeping pills, are a class of psychoactive drugs whose primary function is to induce sleep and to treat insomnia (sleeplessness).

Sir Edward Mellanby was a British biochemist and nutritionist who discovered vitamin D and its role in preventing rickets in 1919.

The Heart Protection Study was a randomized controlled trial run by the Clinical Trial Service Unit, and funded by the Medical Research Council (MRC) and the British Heart Foundation (BHF) in the United Kingdom. It studied the use of the cholesterol lowering drug, simvastatin 40 mg and vitamin supplementation in people who were at risk of cardiovascular disease. It was led by Jane Armitage, an epidemiologist at the Clinical Trial Service Unit.

Atorvastatin is a statin medication used to prevent cardiovascular disease in those at high risk and to treat abnormal lipid levels. For the prevention of cardiovascular disease, statins are a first-line treatment. It is taken by mouth.

Sir Thomas Lauder Brunton, 1st Baronet, was a British physician who is most-closely associated with the use of amyl nitrite to treat angina pectoris.
The Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI) is a cardiology research group founded as a collaboration between two Italian organisations – the Mario Negri Institute for Pharmacological Research and the Associazione Nazionale dei Medici Cardiologi Ospedalieri (ANMCO).

Norpropoxyphene is a major metabolite of the opioid analgesic drug dextropropoxyphene, and is responsible for many of the side effects associated with use of this drug, especially the unusual toxicity seen during dextropropoxyphene overdose. It has weaker analgesic effects than dextropropoxyphene itself, but is a relatively potent pro-convulsant and blocker of sodium and potassium channels, particularly in heart tissue, which produces prolonged intracardiac conduction time and can lead to heart failure following even relatively minor overdoses. The toxicity of this metabolite makes dextropropoxyphene up to 10 times more likely to cause death following overdose compared to other similar mild opioid analgesics, and has led to dextropropoxyphene being withdrawn from the market in some countries.
Donald Robert James Singer was a British clinical pharmacologist who was the president of the Fellowship of Postgraduate Medicine.
Himmatrao Saluba Bawaskar is an Indian physician from Mahad, Maharashtra. He is known for his research on treatment for scorpion stings. Much of his work has been published in the British medical journal The Lancet. He has also conducted research in the fields of snake bites, cardiovascular diseases, and hypothyroidism.
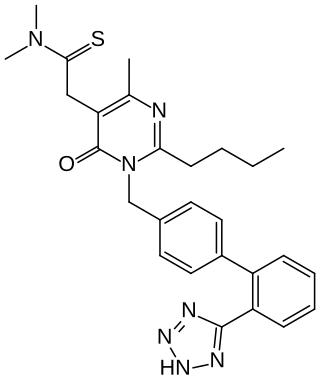
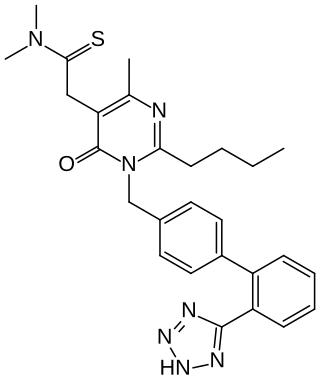
Fimasartan is a non-peptide angiotensin II receptor antagonist (ARB) used for the treatment of hypertension and heart failure. Through oral administration, fimasartan blocks angiotensin II receptor type 1 (AT1 receptors), reducing pro-hypertensive actions of angiotensin II, such as systemic vasoconstriction and water retention by the kidneys. Concurrent administration of fimasartan with diuretic hydrochlorothiazide has shown to be safe in clinical trials. Fimasartan was approved for use in South Korea on September 9, 2010, and is available under the brand name Kanarb through Boryung Pharmaceuticals, who are presently seeking worldwide partnership.

Michael B. Murphy is an Irish doctor and academic. He was the President of University College Cork from 2007 to 2017. From 2019 until 2023, Murphy served as the president of the European University Association (EUA). Since October 2024 he is serving as president of the National University of Ireland.

Sir Derrick Melville Dunlop was a Scottish physician and pharmacologist in British medical administration and policy-making in the late 20th century. Sir Derrick established the Dunlop Committee which investigates the side-effects of new drugs in the UK.
Andrew Herxheimer was a German-born British clinical pharmacologist. He was "interested in all aspects of providing independent, unbiased, clear and concise information about therapeutic interventions to professionals and the public, and [had] a long experience of observing the pharmaceutical industry at work". He is known for founding Drug and Therapeutics Bulletin, to better educate medical providers on prescription drugs. After retiring from his academic career at London Hospital and Charing Cross in 1991, he continued his career as a consultant for the Cochrane Collaboration with a focus on adverse drug effects, and as an internationalist in patient advocacy and consumer advocacy.
The Cameron Prize for Therapeutics of the University of Edinburgh is awarded by the College of Medicine and Veterinary Medicine to a person who has made any highly important and valuable addition to practical therapeutics in the previous five years. The prize, which may be awarded biennially, was founded in 1878 by Andrew Robertson Cameron of Richmond, New South Wales, with a sum of £2,000. The University's senatus academicus may require the prizewinner to deliver one or more lectures or to publish an account on the addition made to practical therapeutics. A list of recipients of the prize dates back to 1879.
Joseph Gavin Collier is a British retired clinical pharmacologist and emeritus professor of medicines policy at St George's Hospital and Medical School in London, whose early research included establishing the effect of aspirin on human prostaglandins and looking at the role of nitric oxide and angiotensin converting enzyme in controlling blood vessel tone and blood pressure. Later, in his national policy work, he helped change the way drugs are priced and bought by the NHS, and ensured that members of governmental advisory committees published their conflicts of interest.
Una Martin is an emeritus professor of clinical pharmacology and was formerly the deputy pro-vice chancellor for equalities at the University of Birmingham. She is an expert in hypertension and ambulatory monitoring. She is a Fellow of the British Pharmacological Society.
Sir Colin Terence Dollery was a clinical pharmacologist who spent much of his life working for SmithKline Beecham and its successor, Glaxo Smith Kline. He was knighted in the Queen's 1987 birthday honours. He was an honorary fellow of the British Pharmacological Society and a fellow of the Academy of Medical Sciences.
Emma Harriet Baker is a British professor of clinical pharmacology and consultant physician in internal medicine at St George's Hospital, London. She has a specialist interest in people who have multiple medical conditions at the same time and take several medications, with a particular focus on lung disease. She is director of the UK's first BSc in clinical pharmacology, clinical vice president of the British Pharmacological Society and training programme director at Health Education England.
Robert Gray Robin Shanks CBE is a British retired clinical pharmacologist, specialising in Beta adrenergic blocking drugs. He was made a Commander of the Order of the British Empire (CBE) in the 1997 New Year Honours, For Services to Medicine.
John Henry Bryant was a British physician, and lecturer on materia medica and therapeutics at Guy's Hospital, London. The blue scrotum sign of Bryant is named after him. In 1903 he had given the first description of abdominal and scrotal bruising in a person with a ruptured abdominal aortic aneurysm.