Related Research Articles
Genetic counseling is the process of investigating individuals and families affected by or at risk of genetic disorders to help them understand and adapt to the medical, psychological and familial implications of genetic contributions to disease. This field is considered necessary for the implementation of genomic medicine. The process integrates:

Genetic testing, also known as DNA testing, is used to identify changes in DNA sequence or chromosome structure. Genetic testing can also include measuring the results of genetic changes, such as RNA analysis as an output of gene expression, or through biochemical analysis to measure specific protein output. In a medical setting, genetic testing can be used to diagnose or rule out suspected genetic disorders, predict risks for specific conditions, or gain information that can be used to customize medical treatments based on an individual's genetic makeup. Genetic testing can also be used to determine biological relatives, such as a child's biological parentage through DNA paternity testing, or be used to broadly predict an individual's ancestry. Genetic testing of plants and animals can be used for similar reasons as in humans, to gain information used for selective breeding, or for efforts to boost genetic diversity in endangered populations.
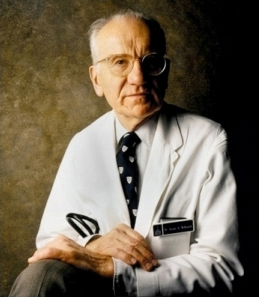
Victor Almon McKusick was an American internist and medical geneticist, and Professor of Medicine at the Johns Hopkins Hospital, Baltimore. He was a proponent of the mapping of the human genome due to its use for studying congenital diseases. He is well known for his studies of the Amish. He was the original author and, until his death, remained chief editor of Mendelian Inheritance in Man (MIM) and its online counterpart Online Mendelian Inheritance in Man (OMIM). He is widely known as the "father of medical genetics".

Pharmacogenomics is the study of the role of the genome in drug response. Its name reflects its combining of pharmacology and genomics. Pharmacogenomics analyzes how the genetic makeup of a patient affects their response to drugs. It deals with the influence of acquired and inherited genetic variation on drug response, by correlating DNA mutations with pharmacokinetic, pharmacodynamic, and/or immunogenic endpoints.

Personalized medicine, also referred to as precision medicine, is a medical model that separates people into different groups—with medical decisions, practices, interventions and/or products being tailored to the individual patient based on their predicted response or risk of disease. The terms personalized medicine, precision medicine, stratified medicine and P4 medicine are used interchangeably to describe this concept though some authors and organisations use these expressions separately to indicate particular nuances.
Genetic discrimination occurs when people treat others differently because they have or are perceived to have a gene mutation(s) that causes or increases the risk of an inherited disorder. It may also refer to any and all discrimination based on the genotype of a person rather than their individual merits, including that related to race, although the latter would be more appropriately included under racial discrimination. Some legal scholars have argued for a more precise and broader definition of genetic discrimination: "Genetic discrimination should be defined as when an individual is subjected to negative treatment, not as a result of the individual's physical manifestation of disease or disability, but solely because of the individual's genetic composition." Genetic Discrimination is considered to have its foundations in genetic determinism and genetic essentialism, and is based on the concept of genism, i.e. distinctive human characteristics and capacities are determined by genes.
The Personal Genome Project (PGP) is a long term, large cohort study which aims to sequence and publicize the complete genomes and medical records of 100,000 volunteers, in order to enable research into personal genomics and personalized medicine. It was initiated by Harvard University's George M. Church in 2005. As of November 2017, more than 10,000 volunteers had joined the project. Volunteers were accepted initially if they were permanent residents of the US and were able to submit tissue and/or genetic samples. Later the project was expanded to other countries.

George McDonald Church is an American geneticist, molecular engineer, chemist, serial entrepreneur, and pioneer in personal genomics and synthetic biology. He is the Robert Winthrop Professor of Genetics at Harvard Medical School, Professor of Health Sciences and Technology at Harvard University and Massachusetts Institute of Technology, and a founding member of the Wyss Institute for Biologically Inspired Engineering at Harvard. Through his Harvard lab Church has co-founded around 50 biotech companies pushing the boundaries of innovation in the world of life sciences and making his lab as a hotbed of biotech startup activity in Boston. In 2018, the Church lab at Harvard made a record by spinning off 16 biotech companies in one year. The Church lab works on research projects that are distributed in diverse areas of modern biology like developmental biology, neurobiology, info processing, medical genetics, genomics, gene therapy, diagnostics, chemistry & bioengineering, space biology & space genetics, and ecosystem. Research and technology developments at the Church lab have impacted or made direct contributions to nearly all "next-generation sequencing (NGS)" methods and companies. In 2017, Time magazine listed him in Time 100, the list of 100 most influential people in the world. In 2022, he was featured among the most influential people in biopharma by Fierce Pharma, and was listed among the top 8 famous geneticists of all time in human history. As of January 2023, Church serves as a member of the Bulletin of the Atomic Scientists' Board of Sponsors, established by Albert Einstein.

In genomics, a genome-wide association study, is an observational study of a genome-wide set of genetic variants in different individuals to see if any variant is associated with a trait. GWA studies typically focus on associations between single-nucleotide polymorphisms (SNPs) and traits like major human diseases, but can equally be applied to any other genetic variants and any other organisms.
Personal genomics or consumer genetics is the branch of genomics concerned with the sequencing, analysis and interpretation of the genome of an individual. The genotyping stage employs different techniques, including single-nucleotide polymorphism (SNP) analysis chips, or partial or full genome sequencing. Once the genotypes are known, the individual's variations can be compared with the published literature to determine likelihood of trait expression, ancestry inference and disease risk.
Population genomics is the large-scale comparison of DNA sequences of populations. Population genomics is a neologism that is associated with population genetics. Population genomics studies genome-wide effects to improve our understanding of microevolution so that we may learn the phylogenetic history and demography of a population.

Whole genome sequencing (WGS), also known as full genome sequencing, complete genome sequencing, or entire genome sequencing, is the process of determining the entirety, or nearly the entirety, of the DNA sequence of an organism's genome at a single time. This entails sequencing all of an organism's chromosomal DNA as well as DNA contained in the mitochondria and, for plants, in the chloroplast.
Paul Billings is an American doctor, lecturer, researcher, professor, and consultant on genetic information. His major research interests include the impact of genomic information and biotechnology on society, the integration of genomics and diagnostics in to health and medical care and individualized genomic medicine. Dr. Paul Billings is the author of more than 250 publications and books on genomic medicine, has spoken at numerous medical conferences, and appeared on talk shows such as The Oprah Show and 60 Minutes. He is currently the chief medical officer of Natera, chairman of Biological Dynamics, Inc. and Plumcare LLC, and CEO of Synergenz Bioscience, Inc.
Genomic counseling is the process by which a person gets informed about his or her genome often in the setting of elective genetic and genomic testing. In contrast to genetic counseling, which focuses on Mendelian diseases and typically involves person-to-person communication with a genetic counselor or other medical genetics expert, genomic counseling is not limited to currently clinically relevant information. It is often based on genomic information that is of interest for the informed person, such as increased risk for common complex disease that has actionable components, genetically determined non-disease related traits, or recreational forms of information and genetic genealogy data. An individual's response to certain medications/drugs based on their pharmacogenomic profile may be provided.

Robert C. Green is an American medical geneticist, physician, and public health researcher. He directs the Genomes2People Research Program in translational genomics and health outcomes in the Division of Genetics at Brigham and Women's Hospital and the Broad Institute, and is Director of the Preventive Genomics Clinic at Brigham and Women's Hospital. Research led by Green includes clinical and research aspects of genomic and precision medicine, including the development and disclosure of Alzheimer's disease risk estimates and one of the first prospective studies of direct-to-consumer genetic testing services. He has studied the implementation of medical sequencing in healthy adults, newborns, and active duty military personnel. As of 2020, he is leading the first research collaboration to explore return of genomic results and better understand penetrance in a population-based cohort of underrepresented minorities. He has led the Preventive Genomics Clinic at Brigham and Women's Hospital since its creation in 2019.

The Personal Genetics Education Project (pgEd) aims to engage and inform a worldwide audience about the benefits of knowing one's genome as well as the ethical, legal and social issues (ELSI) and dimensions of personal genetics. pgEd was founded in 2006, is housed in the Department of Genetics at Harvard Medical School and is directed by Ting Wu, a professor in that department. It employs a variety of strategies for reaching general audiences, including generating online curricular materials, leading discussions in classrooms, workshops, and conferences, developing a mobile educational game (Map-Ed), holding an annual conference geared toward accelerating awareness (GETed), and working with the world of entertainment to improve accuracy and outreach.

Chao-ting Wu is an American molecular biologist. After training at Harvard Medical School in genetics with William Gelbart, at Stanford Medical School with David Hogness, and in a fellowship at Massachusetts General Hospital in molecular biology, Wu began her independent academic career as an assistant professor in Anatomy and Cellular Biology and then Genetics at Harvard Medical School in 1993. After a period as Professor of Pediatrics in the Division of Molecular Medicine at the Boston Children's Hospital, she returned to the Department of Genetics at Harvard Medical School as a full professor in 2007.
Predictive genomics is at the intersection of multiple disciplines: predictive medicine, personal genomics and translational bioinformatics. Specifically, predictive genomics deals with the future phenotypic outcomes via prediction in areas such as complex multifactorial diseases in humans. To date, the success of predictive genomics has been dependent on the genetic framework underlying these applications, typically explored in genome-wide association (GWA) studies. The identification of associated single-nucleotide polymorphisms underpin GWA studies in complex diseases that have ranged from Type 2 Diabetes (T2D), Age-related macular degeneration (AMD) and Crohn's disease.
Elective genetic and genomic testing are DNA tests performed for an individual who does not have an indication for testing. An elective genetic test analyzes selected sites in the human genome while an elective genomic test analyzes the entire human genome. Some elective genetic and genomic tests require a physician to order the test to ensure that individuals understand the risks and benefits of testing as well as the results. Other DNA-based tests, such as a genealogical DNA test do not require a physician's order. Elective testing is generally not paid for by health insurance companies. With the advent of personalized medicine, also called precision medicine, an increasing number of individuals are undertaking elective genetic and genomic testing.
Personalized genomics is the human genetics-derived study of analyzing and interpreting individualized genetic information by genome sequencing to identify genetic variations compared to the library of known sequences. International genetics communities have spared no effort from the past and have gradually cooperated to prosecute research projects to determine DNA sequences of the human genome using DNA sequencing techniques. The methods that are the most commonly used are whole exome sequencing and whole genome sequencing. Both approaches are used to identify genetic variations. Genome sequencing became more cost-effective over time, and made it applicable in the medical field, allowing scientists to understand which genes are attributed to specific diseases.
References
- 1 2 3 Lamb, N. E.; Myers, R. M.; Gunter, C. (2009). "Education and personalized genomics: Deciphering the public's genetic health report". Personalized Medicine. 6 (6): 681–690. doi:10.2217/pme.09.57. PMC 2821046 . PMID 20161675.
- 1 2 3 Salari, K. (2009). "The Dawning Era of Personalized Medicine Exposes a Gap in Medical Education". PLOS Medicine. 6 (8): e1000138. doi: 10.1371/journal.pmed.1000138 . PMC 2719811 . PMID 19707267.
- 1 2 McKinnon, R.; Anderson, C. (2011). "Transforming Pharmaceutical Education to Accelerate the Acceptance and Implementation of Personalized Medicine". American Journal of Pharmaceutical Education. 75 (6): 107. doi:10.5688/ajpe756107. PMC 3175667 . PMID 21931445.
- 1 2 3 Salari, K.; Pizzo, P. A.; Prober, C. G. (2011). "Commentary: To Genotype or Not to Genotype? Addressing the Debate Through the Development of a Genomics and Personalized Medicine Curriculum". Academic Medicine. 86 (8): 925–927. doi: 10.1097/ACM.0b013e3182223acf . PMID 21795901.
- ↑ Robertson, J. A. (2003). "The $1000 Genome: Ethical and Legal Issues in Whole Genome Sequencing of Individuals". The American Journal of Bioethics. 3 (3): 35–36. doi:10.1162/152651603322874762. PMID 14735880. S2CID 15357657.
- ↑ Thurston, V. C.; Wales, P. S.; Bell, M. A.; Torbeck, L.; Brokaw, J. J. (2007). "The Current Status of Medical Genetics Instruction in U.S. And Canadian Medical Schools". Academic Medicine. 82 (5): 441–445. doi: 10.1097/ACM.0b013e31803e86c5 . PMID 17457062.
- ↑ Kathryn Roethel (July 12, 2010). "Stanford genotype class asks: What's your type?". SFGate. Retrieved 14 May 2013.
- 1 2 3 Ferris Jabr (September 24, 2012). "Exposing the Student Body: Stanford Joins U.C. Berkeley in Controversial Genetic Testing of Students". Scientific American. Retrieved 14 May 2013.
- ↑ Vernez, S.; Salari, K.; Ormond, K. E.; Lee, S. S. O. J. N. (2013). "Personal genome testing in medical education: Student experiences with genotyping in the classroom". Genome Medicine. 5 (3): 24. doi: 10.1186/gm428 . PMC 3706781 . PMID 23510111.
- ↑ "Student Physician, Sequence Thyself". Genome Web Daily News. October 10, 2012. Retrieved 14 May 2013.
- ↑ Monya Baker (October 11, 2012). "Personal genomics in the classroom: Students sequence themselves". Nature News Blog. Retrieved 14 May 2013.
- 1 2 "A DNA education". Nature. 465 (7300): 845–846. June 16, 2010. Bibcode:2010Natur.465R.845.. doi: 10.1038/465845b . PMID 20559338 . Retrieved 14 May 2013.
- ↑ Tamar Lewin (May 18, 2010). "College bound, DNA swab in hand". Nature. Retrieved 14 May 2013.
- ↑ Rachel Gross (August 11, 2010). "UC Berkeley DNA testing goes before state committee". Berkeleyside. Retrieved 14 May 2013.
- ↑ "California Legislation Seeks to Bar UC Berkeley's Genetic Testing Plans". Genome Web Daily News. July 14, 2010. Retrieved 14 May 2013.
- ↑ Alla Katsnelson (August 12, 2010). "State halts UC Berkeley's gene testing plans". Nature News Blog. Retrieved 14 May 2013.
- ↑ Gina Shaw (February 2012). "The Right Type: Personal Genetic Testing in the Medical School Curriculum". AAMC Reporter. Retrieved 14 May 2013.