An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.

An intracranial aneurysm, also known as a cerebral aneurysm, is a cerebrovascular disorder characterized by a localized dilation or ballooning of a blood vessel in the brain due to a weakness in the vessel wall. These aneurysms can occur in any part of the brain but are most commonly found in the arteries of the cerebral arterial circle. The risk of rupture varies with the size and location of the aneurysm, with those in the posterior circulation being more prone to rupture.

Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. Modern angiography is performed by injecting a radio-opaque contrast agent into the blood vessel and imaging using X-ray based techniques such as fluoroscopy. With time-of-flight (TOF) magnetic ressonance it is no longer necessary to use a contrast.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.
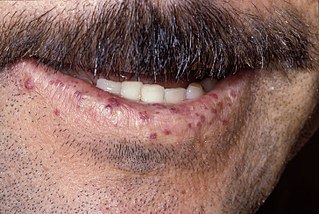
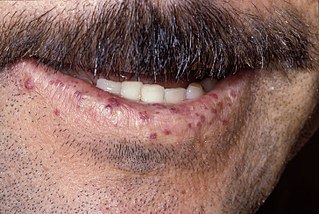
Hereditary hemorrhagic telangiectasia (HHT), also known as Osler–Weber–Rendu disease and Osler–Weber–Rendu syndrome, is a rare autosomal dominant genetic disorder that leads to abnormal blood vessel formation in the skin, mucous membranes, and often in organs such as the lungs, liver, and brain.

Cerebral angiography is a form of angiography which provides images of blood vessels in and around the brain, thereby allowing detection of abnormalities such as arteriovenous malformations and aneurysms. It was pioneered in 1927 by the Portuguese neurologist Egas Moniz at the University of Lisbon, who also helped develop thorotrast for use in the procedure.
Transcatheter arterial chemoembolization (TACE) is a minimally invasive procedure performed in interventional radiology to restrict a tumor's blood supply. Small embolic particles coated with chemotherapeutic drugs are injected selectively through a catheter into an artery directly supplying the tumor. These particles both block the blood supply and induce cytotoxicity, attacking the tumor in several ways.

Uterine artery embolization is a procedure in which an interventional radiologist uses a catheter to deliver small particles that block the blood supply to the uterine body. The procedure is primarily done for the treatment of uterine fibroids and adenomyosis. Compared to surgical treatment for fibroids such as a hysterectomy, in which a woman's uterus is removed, uterine artery embolization may be beneficial in women who wish to retain their uterus. Other reasons for uterine artery embolization are postpartum hemorrhage and uterine arteriovenous malformations.

Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radionuclide therapy used in interventional radiology to treat cancer. It is generally for selected patients with surgically unresectable cancers, especially hepatocellular carcinoma or metastasis to the liver. The treatment involves injecting tiny microspheres of radioactive material into the arteries that supply the tumor, where the spheres lodge in the small vessels of the tumor. Because this treatment combines radiotherapy with embolization, it is also called radioembolization. The chemotherapeutic analogue is called chemoembolization, of which transcatheter arterial chemoembolization (TACE) is the usual form.
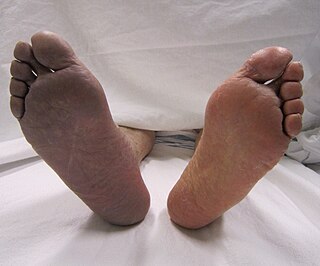
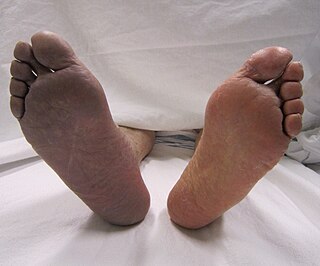
Acute limb ischaemia (ALI) occurs when there is a sudden lack of blood flow to a limb within 14 days of symptoms onset. On the other hand, when the symptoms exceed 14 days, it is called critical limb ischemia (CLI). CLI is the end stage of peripheral vascular disease where there is still some collateral circulation that bring some blood flow to the distal parts of the limbs. While limbs in both acute and chronic limb ischemia may be pulseless, a chronically ischemic limb is typically warm and pink due to a well-developed collateral artery network and does not need emergency intervention to avoid limb loss, whereas ALI is a vascular emergency.
Interventional neuroradiology (INR) also known as neurointerventional surgery (NIS), endovascular therapy (EVT), endovascular neurosurgery, and interventional neurology is a medical subspecialty of neurosurgery, neuroradiology, intervention radiology and neurology specializing in minimally invasive image-based technologies and procedures used in diagnosis and treatment of diseases of the head, neck, and spine.
Hepatic artery embolization, also known as trans-arterial embolization (TAE), is one of the several therapeutic methods to treat primary liver tumors or metastases to the liver. The embolization therapy can reduce the size of the tumor, and decrease the tumor's impact such its hormone production, effectively decreasing symptoms. The treatment was initially developed in the early 1970s. The several types of hepatic artery treatments are based on the observation that tumor cells get nearly all their nutrients from the hepatic artery, while the normal cells of the liver get about 70-80 percent of their nutrients and 50% their oxygen supply from the portal vein, and thus can survive with the hepatic artery effectively blocked. In practice, hepatic artery embolization occludes the blood flow to the tumors, achieving significant tumor shrinkage in over 80% of people. Shrinkage rates vary.
Interventional oncology is a subspecialty field of interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments to allow targeted and precise treatment of solid tumours located in various organs of the human body, including but not limited to the liver, kidneys, lungs, and bones. Interventional oncology treatments are routinely carried out by interventional radiologists in appropriate settings and facilities.
Portal vein embolization (PVE) is a preoperative procedure performed in interventional radiology to initiate hypertrophy of the anticipated future liver remnant a couple weeks prior to a major liver resection procedure. The procedure involves injecting the right or left portal vein with embolic material to occlude portal blood flow. By occluding the blood flow to areas of the liver that will be resected away, the blood is diverted to healthy parts of the liver and induces hyperplasia. This may allow for a more extensive resection or stage bilateral resections that would otherwise be contraindicated resulting in better oncological treatment outcomes.
Endovascular and hybrid trauma and bleeding management is a new and rapidly evolving concept within medical healthcare and endovascular resuscitation. It involves early multidisciplinary evaluation and management of hemodynamically unstable patients with traumatic injuries as well as being a bridge to definitive treatment. It has recently been shown that the EVTM concept may also be applied to non-traumatic hemodynamically unstable patients.
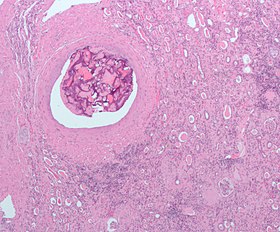
Transarterial bland embolization is a catheter-based tumor treatment of the liver. In this procedure, embolizing agents can be delivered through the tumor's feeding artery in order to completely occlude the tumor's blood supply. The anti-tumor effects are solely based on tumor ischemia and infarction of tumor tissue, as no chemotherapeutic agents are administered. The rationale for the use of bland embolization for hepatocellular carcinoma (HCC) and/or other hyper-vascular tumors is based on the fact that a normal liver receives a dual blood supply from the hepatic artery (25%) and the portal vein (75%). As the tumor grows, it becomes increasingly dependent on the hepatic artery for blood supply. Once a tumor nodule reaches a diameter of 2 cm or more, most of the blood supply is derived from the hepatic artery. Therefore, bland embolization and transarterial chemoembolization (TACE) consist of the selective angiographic occlusion of the tumor arterial blood supply with a variety of embolizing agents, with or without the precedence of local chemotherapy infusion. The occlusion by embolic particles results in tumor hypoxia and necrosis, without affecting the normal hepatic parenchyma.
Segmental arterial mediolysis (SAM) is a rare disorder of the arteries characterized by the development of aneurysms, blood clots, narrowing of the arteries (stenoses), and blood collections (hematomas) in the affected distribution.
Bronchial artery embolization is a treatment for hemoptysis, abbreviated as BAE. It is a kind of catheter intervention to control hemoptysis by embolizing the bronchial artery, which is a bleeding source. Embolic agents are particulate embolic material such as gelatin sponge or polyvinyl alcohol (PVA), and liquid embolic material such as NBCA, or metallic coils.

Arterial occlusion is a condition involving partial or complete blockage of blood flow through an artery. Arteries are blood vessels that carry oxygenated blood to body tissues. An occlusion of arteries disrupts oxygen and blood supply to tissues, leading to ischemia. Depending on the extent of ischemia, symptoms of arterial occlusion range from simple soreness and pain that can be relieved with rest, to a lack of sensation or paralysis that could require amputation.

Hemorrhoidal artery embolization is a non-surgical treatment of internal hemorrhoids.