Related Research Articles

Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults and is currently the most common cause of death in people with cirrhosis. HCC is the third leading cause of cancer-related deaths worldwide.
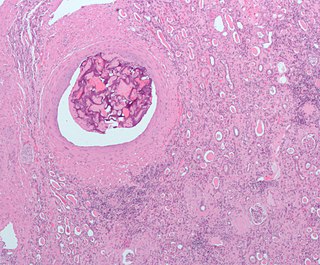
Liver tumors are abnormal growth of liver cells on or in the liver. Several distinct types of tumors can develop in the liver because the liver is made up of various cell types. Liver tumors can be classified as benign (non-cancerous) or malignant (cancerous) growths. They may be discovered on medical imaging, and the diagnosis is often confirmed with liver biopsy. Signs and symptoms of liver masses vary from being asymptomatic to patients presenting with an abdominal mass, hepatomegaly, abdominal pain, jaundice, or some other liver dysfunction. Treatment varies and is highly specific to the type of liver tumor.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.
Embolization refers to the passage and lodging of an embolus within the bloodstream. It may be of natural origin (pathological), in which sense it is also called embolism, for example a pulmonary embolism; or it may be artificially induced (therapeutic), as a hemostatic treatment for bleeding or as a treatment for some types of cancer by deliberately blocking blood vessels to starve the tumor cells.

Sorafenib, sold under the brand name Nexavar, is a kinase inhibitor drug approved for the treatment of primary kidney cancer, advanced primary liver cancer, FLT3-ITD positive AML and radioactive iodine resistant advanced thyroid carcinoma.
Iodized oil, also known as ethiodized oil, brand name Lipiodol, is a medication derived from poppyseed oil and iodine. When given by injection, it is a radio-opaque contrast agent that is used to outline structures in radiological investigations. When given orally or by intramuscular injection once or twice a year, it prevents endemic goitre in remote communities. It has an additional use in gastric variceal obliteration as a dilutant that does not affect polymerization of cyanoacrylate.

Sirtex Medical Limited is a medical device firm that offers radioactive treatment for inoperable liver cancer called SIR-Spheres microspheres. Sirtex was founded in 1997 in Australia and today has offices and production facilities in the U.S., Australia, Germany, and Singapore. Following its acquisition by China Grand Pharmaceutical and CDH Genetech, Sirtex delisted from the Australian Securities Exchange (ASX:SRX) on Monday, September 24, 2018.

Liver cancer, also known as hepatic cancer, primary hepatic cancer, or primary hepatic malignancy, is cancer that starts in the liver. Liver cancer can be primary in which the cancer starts in the liver, or it can be liver metastasis, or secondary, in which the cancer spreads from elsewhere in the body to the liver. Liver metastasis is the more common of the two liver cancers. Instances of liver cancer are increasing globally.
TheraSphere is a radiotherapy treatment for hepatocellular carcinoma (HCC) that consists of millions of microscopic, radioactive glass microspheres being infused into the arteries that feed liver tumors. These microspheres then embolize, lodging themselves in the liver's capillaries and bathing the malignancy in high levels of yttrium-90 radiation. It is currently approved as a Humanitarian Device, meaning effectiveness has not been proven, for patients as a neoadjuvant to surgery or transplantation by the U.S. Food and Drug Administration and is being used at a number of clinical centers in the United States.
Hepatic arterial infusion (HAI) is a medical procedure that delivers chemotherapy directly to the liver. The procedure, mostly used in combination with systemic chemotherapy, plays a role in the treatment of liver metastases in patients with colorectal cancer (CRC). Although surgical resection remains the standard of care for these liver metastases, majority of patients have lesions that are unresectable.

Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radionuclide therapy used in interventional radiology to treat cancer. It is generally for selected patients with surgically unresectable cancers, especially hepatocellular carcinoma or metastasis to the liver. The treatment involves injecting tiny microspheres of radioactive material into the arteries that supply the tumor, where the spheres lodge in the small vessels of the tumor. Because this treatment combines radiotherapy with embolization, it is also called radioembolization. The chemotherapeutic analogue is called chemoembolization, of which transcatheter arterial chemoembolization (TACE) is the usual form.
Yttrium-90 is a radioactive isotope of yttrium. Yttrium-90 has found a wide range of uses in radiation therapy to treat some forms of cancer. Along with other isotopes of yttrium, it is sometimes called radioyttrium.

Brivanib alaninate (INN/USAN) also known as BMS-582664 is an investigational, anti-tumorigenic drug for oral administration. The drug is being developed by Bristol-Myers Squibb for the treatment of hepatocellular carcinoma or HCC, the most common type of liver cancer. Brivanib is no longer in active development.
Hepatic artery embolization, also known as trans-arterial embolization (TAE), is one of the several therapeutic methods to treat primary liver tumors or metastases to the liver. The embolization therapy can reduce the size of the tumor, and decrease the tumor's impact such its hormone production, effectively decreasing symptoms. The treatment was initially developed in the early 1970s. The several types of hepatic artery treatments are based on the observation that tumor cells get nearly all their nutrients from the hepatic artery, while the normal cells of the liver get about 70-80 percent of their nutrients and 50% their oxygen supply from the portal vein, and thus can survive with the hepatic artery effectively blocked. In practice, hepatic artery embolization occludes the blood flow to the tumors, achieving significant tumor shrinkage in over 80% of people. Shrinkage rates vary.
Interventional oncology is a subspecialty field of interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments to allow targeted and precise treatment of solid tumours located in various organs of the human body, including but not limited to the liver, kidneys, lungs, and bones. Interventional oncology treatments are routinely carried out by interventional radiologists in appropriate settings and facilities.
Radiation lobectomy is a form of radiation therapy used in interventional radiology to treat liver cancer. It is performed in patients that would be surgical candidates for resection, but cannot undergo surgery due to insufficient remaining liver tissue. It consists of injecting small radioactive beads loaded with yttrium-90 into the hepatic artery feeding the hepatic lobe in which the tumor is located. This is done with the intent of inducing growth in the contralateral hepatic lobe, not dissimilarly from portal vein embolization (PVE).
Ultrasonography of liver tumors involves two stages: detection and characterization.
Transarterial bland embolization is a catheter-based tumor treatment of the liver. In this procedure, embolizing agents can be delivered through the tumor's feeding artery in order to completely occlude the tumor's blood supply. The anti-tumor effects are solely based on tumor ischemia and infarction of tumor tissue, as no chemotherapeutic agents are administered. The rationale for the use of bland embolization for hepatocellular carcinoma (HCC) and/or other hyper-vascular tumors is based on the fact that a normal liver receives a dual blood supply from the hepatic artery (25%) and the portal vein (75%). As the tumor grows, it becomes increasingly dependent on the hepatic artery for blood supply. Once a tumor nodule reaches a diameter of 2 cm or more, most of the blood supply is derived from the hepatic artery. Therefore, bland embolization and transarterial chemoembolization (TACE) consist of the selective angiographic occlusion of the tumor arterial blood supply with a variety of embolizing agents, with or without the precedence of local chemotherapy infusion. The occlusion by embolic particles results in tumor hypoxia and necrosis, without affecting the normal hepatic parenchyma.

Liver angiosarcoma also known as angiosarcoma of the liver or hepatic angiosarcoma is a rare and rapidly fatal cancer arising from endothelial that line the blood vessels of the liver. It is a type of angiosarcoma. Although very rare with around 200 cases diagnosed each year, it is still considered the third most common primary liver cancer, making up around 2% of all primary liver cancers. Liver angiosarcoma can be primary, meaning it arose in the liver, or secondary, meaning the angiosarcoma arose elsewhere and metastasized to the liver. This article covers PHA, however much is also applicable to secondary tumors.

Miriplatin is a drug used to treat hepatocellular carcinoma (HCC). It is a lipophilic platinum complex that is used in transcatheter arterial chemoembolization (TACE). Miriplatin was approved by Japan's Pharmaceuticals and Medical Devices Agency in 2009.
References
- 1 2 3 4 5 6 7 Raoul JL, Forner A, Bolondi L, Cheung TT, Kloeckner R, de Baere T (January 2019). "Updated use of TACE for hepatocellular carcinoma treatment: How and when to use it based on clinical evidence". Cancer Treat Rev. 72: 28–36. doi:10.1016/j.ctrv.2018.11.002. PMID 30447470.
- ↑ Young, Michael; John, Savio (2023), "Hepatic Chemoembolization", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29939599 , retrieved 2023-11-24
- ↑ Miraglia R, Pietrosi G, Maruzzelli L, et al. (2007). "Efficacy of transcatheter embolization/chemoembolization (TAE/TACE) for the treatment of single hepatocellular carcinoma". World J Gastroenterol. 13 (21): 2952–5. doi: 10.3748/wjg.v13.i21.2952 . PMC 4171147 . PMID 17589945.
- ↑ Rammohan A, Sathyanesan J, Ramaswami S, et al. (2012). "Embolization of liver tumors: Past, present and future". World Journal of Radiology. 4 (9): 405–12. doi: 10.4329/wjr.v4.i9.405 . PMC 3460228 . PMID 23024842.
- ↑ Brown DB, Geschwind JF, Soulen MC, Millward SF, Sacks D (2006). "Society of Interventional Radiology position statement on chemoembolization of hepatic malignancies". J Vasc Interv Radiol. 17 (2): 217–23. doi: 10.1097/01.rvi.0000196277.76812.a3 . PMID 16517767.
- ↑ Miyayama, Shiro. "Applying Superselective Conventional TACE". Endovascular Today. Retrieved 2023-05-26.
- ↑ Walker, Sandra Beverley; Cleary, Sonja; Higgins, Monica (December 2001). "Comparison of the FemoStop device and manual pressure in reducing groin puncture site complications following coronary angioplasty and coronary stent placement". International Journal of Nursing Practice. 7 (6): 366–375. doi:10.1046/j.1440-172x.2001.00291.x. ISSN 1322-7114. PMID 11785439.
- ↑ Guan, YS; He, Q; Wang, MQ (2012). "Transcatheter arterial chemoembolization: history for more than 30 years". ISRN Gastroenterology. 2012: 480650. doi: 10.5402/2012/480650 . PMC 3433134 . PMID 22966466. S2CID 15761122.
- ↑ Mikhail AS, Negussie AH, Mauda-Havakuk M, Owen JW, Pritchard WF, Lewis AL, Wood BJ (March 2021). "Drug-eluting embolic microspheres: State-of-the-art and emerging clinical applications". Expert Opin Drug Deliv. 18 (3): 383–398. doi:10.1080/17425247.2021.1835858. PMC 11247414 . PMID 33480306.
- ↑ "EmboCept S - the universal short-term embolizate" (PDF). The Spanish Society of Vascular and Interventional Radiology (SERVEI). Archived from the original (PDF) on 12 March 2022. Retrieved 12 March 2022.
- 1 2 3 4 5 6 Hulin A, Stocco J, Bouattour M (August 2019). "Clinical Pharmacokinetics and Pharmacodynamics of Transarterial Chemoembolization and Targeted Therapies in Hepatocellular Carcinoma". Clin Pharmacokinet. 58 (8): 983–1014. doi:10.1007/s40262-019-00740-w. PMID 31093928.
- ↑ Sacco R, Tapete G, Simonetti N, Sellitri R, Natali V, Melissari S, Cabibbo G, Biscaglia L, Bresci G, Giacomelli L (2017). "Transarterial chemoembolization for the treatment of hepatocellular carcinoma: a review". J Hepatocell Carcinoma. 4: 105–110. doi: 10.2147/JHC.S103661 . PMC 5538681 . PMID 28795053.
- ↑ Eugen K (2020). "Current treatment options for hepatocellular carcinoma". Klin Onkol. 33 (Supplementum 3): 20–25. doi:10.14735/amko20203S20. PMID 33213161.
- ↑ Boas FE, Kemeny NE, Sofocleous CT, Yeh R, Thompson VR, Hsu M, Moskowitz CS, Ziv E, Yarmohammadi H, Bendet A, Solomon SB (2021). "Bronchial or Pulmonary Artery Chemoembolization for Unresectable and Unablatable Lung Metastases: A Phase I Clinical Trial". Radiology. 301 (2): 474–84. doi:10.1148/radiol.2021210213. PMC 8574062 . PMID 34463550.
- ↑ Gao F, Gao J, Wang K, Song L (2022). "Efficacy and safety of transarterial chemoembolization with CalliSpheres Microspheres in head and neck cancer". Frontiers in Surgery. 9: 938305. doi: 10.3389/fsurg.2022.938305 . PMC 9452835 . PMID 36090318.
- ↑ Stuart K (2003). "Chemoembolization in the management of liver tumors". Oncologist. 8 (5): 425–37. doi: 10.1634/theoncologist.8-5-425 . PMID 14530495. S2CID 38536397.
- ↑ Guan, YS; He, Q; Wang, MQ (2012). "Transcatheter arterial chemoembolization: history for more than 30 years". ISRN Gastroenterology. 2012: 480650. doi: 10.5402/2012/480650 . PMC 3433134 . PMID 22966466. S2CID 15761122.
- ↑ Guan YS, He Q, Wang MQ (2012). "Transcatheter arterial chemoembolization: history for more than 30 years". ISRN Gastroenterology. 2012: 1–8. doi: 10.5402/2012/480650 . PMC 3433134 . PMID 22966466.