Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system. Symptoms may include a lump in the testicle, or swelling or pain in the scrotum. Treatment may result in infertility.

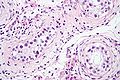
Leydig cells, also known as interstitial cells of Leydig, are found adjacent to the seminiferous tubules in the testicle. They produce testosterone in the presence of luteinizing hormone (LH). Leydig cells are polyhedral in shape, and have a large prominent nucleus, an eosinophilic cytoplasm and numerous lipid-filled vesicles.

Spermatogenesis is the process by which haploid spermatozoa develop from germ cells in the seminiferous tubules of the testis. This process starts with the mitotic division of the stem cells located close to the basement membrane of the tubules. These cells are called spermatogonial stem cells. The mitotic division of these produces two types of cells. Type A cells replenish the stem cells, and type B cells differentiate into primary spermatocytes. The primary spermatocyte divides meiotically into two secondary spermatocytes; each secondary spermatocyte divides into two equal haploid spermatids by Meiosis II. The spermatids are transformed into spermatozoa (sperm) by the process of spermiogenesis. These develop into mature spermatozoa, also known as sperm cells. Thus, the primary spermatocyte gives rise to two cells, the secondary spermatocytes, and the two secondary spermatocytes by their subdivision produce four spermatozoa and four haploid cells.

A Sertoli cell is a "nurse" cell of the testicles that is part of a seminiferous tubule and helps in the process of spermatogenesis, the production of sperm.

Sex cord–gonadal stromal tumour is a group of tumors derived from the stromal component of the ovary and testis, which comprises the granulosa, thecal cells and fibrocytes. In contrast, the epithelial cells originate from the outer epithelial lining surrounding the gonad while the germ cell tumors arise from the precursor cells of the gametes, hence the name germ cell. In humans, this group accounts for 8% of ovarian cancers and under 5% of testicular cancers. Their diagnosis is histological: only a biopsy of the tumour can make an exact diagnosis. They are often suspected of being malignant prior to operation, being solid ovarian tumours that tend to occur most commonly in post menopausal women.

Germ cell tumor (GCT) is a neoplasm derived from germ cells. Germ-cell tumors can be cancerous or benign. Germ cells normally occur inside the gonads. GCTs that originate outside the gonads may be birth defects resulting from errors during development of the embryo.

A seminoma is a germ cell tumor of the testicle or, more rarely, the mediastinum or other extra-gonadal locations. It is a malignant neoplasm and is one of the most treatable and curable cancers, with a survival rate above 95% if discovered in early stages.

Embryonal carcinoma is a relatively uncommon type of germ cell tumour that occurs in the ovaries and testes.

Testicular microlithiasis is an unusual condition diagnosed on testicular ultrasound. It is found in between 1.5 to 5% of normal males, and may be found in up to 20% of individuals with subfertility. It is an asymptomatic, non-progressive disease.

A germinoma is a type of germ-cell tumor, which is not differentiated upon examination. It may be benign or malignant.
Sertoli cell-only syndrome is a disorder characterized by male sterility without sexual abnormality. It describes a condition of the testes in which only Sertoli cells line is present in seminiferous tubules.
Gonocytes are the precursors of spermatogonia that differentiate in the testis from primordial germ cells around week 7 of embryonic development and exist up until the postnatal period, when they become spermatogonia. Despite some uses of the term to refer to the precursors of oogonia, it was generally restricted to male germ cells. Germ cells operate as vehicles of inheritance by transferring genetic and epigenetic information from one generation to the next. Male fertility is centered around continual spermatogonia which is dependent upon a high stem cell population. Thus, the function and quality of a differentiated sperm cell is dependent upon the capacity of its originating spermatogonial stem cell (SSC).

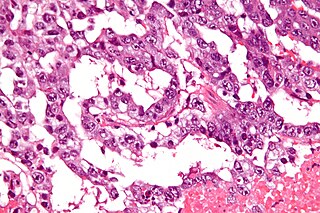
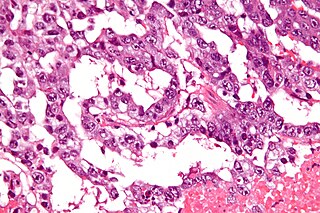
Lobular carcinoma in situ (LCIS) is an incidental microscopic finding with characteristic cellular morphology and multifocal tissue patterns. The condition is a laboratory diagnosis and refers to unusual cells in the lobules of the breast. The lobules and acini of the terminal duct-lobular unit (TDLU), the basic functional unit of the breast, may become distorted and undergo expansion due to the abnormal proliferation of cells comprising the structure. These changes represent a spectrum of atypical epithelial lesions that are broadly referred to as lobular neoplasia (LN).

Spermatocytic tumor, previously called spermatocytic seminoma, is a neoplasm of the testis, and classified as a germ cell tumour.

A Sertoli cell tumour, also Sertoli cell tumor, is a sex cord-gonadal stromal tumor of Sertoli cells. They can occur in the testis or ovary. They are very rare and generally peak between the ages of 35 and 50. They are typically well-differentiated, and may be misdiagnosed as seminomas as they often appear very similar.

Leydig cell tumour, also Leydig cell tumor, (testicular) interstitial cell tumour and (testicular) interstitial cell tumor, is a member of the sex cord-stromal tumour group of ovarian and testicular cancers. It arises from Leydig cells. While the tumour can occur at any age, it occurs most often in young adults.
FNA Mapping is an application of fine-needle aspiration (FNA) to the testis for the diagnosis of male infertility. FNA cytology has been used to examine pathological human tissue from various organs for over 100 years. As an alternative to open testicular biopsy for the last 40 years, FNA Mapping has helped to characterize states of human male infertility due to defective spermatogenesis. Although recognized as a reliable, and informative technique, testis FNA has not been widely used in U.S. to evaluate male infertility. Recently however, testicular FNA has gained popularity as both a diagnostic and therapeutic tool for the management of clinical male infertility for several reasons:
- The testis is an ideal organ for evaluation by FNA because of its uniform cellularity and easy accessibility.
- The trend toward minimally invasive procedures and cost-containment views FNA favorably compared to surgical testis biopsy.
- The realization that the specific histologic abnormality observed on testis biopsy has no definite correlation to either the etiology of infertility or to the ability to find sperm for assisted reproduction.
- Assisted reproduction has undergone dramatic advances such that testis sperm are routinely used for biological pregnancies, thus fueling the development of novel FNA techniques to both locate and procure sperm.

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.
Testicular dysgenesis syndrome is a male reproduction-related condition characterized by the presence of symptoms and disorders such as hypospadias, cryptorchidism, poor semen quality, and testicular cancer. The concept was first introduced by N.E. Skakkaebaek in a research paper along with the department of Growth and Reproduction in Copenhagen University. The paper suggests the origin and underlying cause of TDS can be detected as early as in fetal life, where environmental and genomic factors could affect the development of the male reproductive system.
An Extracranial Germ-Cell Tumor (EGCT) occurs in the abnormal growth of germ cells in the gonads and the areas other than the brain via tissue, lymphatic system, or circulatory system. The tumor can be benign or malignant (cancerous) by its growth rate. According to the National Cancer Institute and St. Jude Children's Research Hospital, the chance of children who are under 15 years old having EGCTs is 3%, in comparison to adolescents, a possibility of 14% with aged 15 to 19 can have EGCTs. There is no obvious cut point in between children and adolescents. However, common cut points in researches are 11 years old and 15 years old.