Adenocarcinoma is a type of cancerous tumor that can occur in several parts of the body. It is defined as neoplasia of epithelial tissue that has glandular origin, glandular characteristics, or both. Adenocarcinomas are part of the larger grouping of carcinomas, but are also sometimes called by more precise terms omitting the word, where these exist. Thus invasive ductal carcinoma, the most common form of breast cancer, is adenocarcinoma but does not use the term in its name—however, esophageal adenocarcinoma does to distinguish it from the other common type of esophageal cancer, esophageal squamous cell carcinoma. Several of the most common forms of cancer are adenocarcinomas, and the various sorts of adenocarcinoma vary greatly in all their aspects, so that few useful generalizations can be made about them.

Cervical intraepithelial neoplasia (CIN), also known as cervical dysplasia, is the abnormal growth of cells on the surface of the cervix that could potentially lead to cervical cancer. More specifically, CIN refers to the potentially precancerous transformation of cells of the cervix.

Prostatic acid phosphatase (PAP), also prostatic specific acid phosphatase (PSAP), is an enzyme produced by the prostate. It may be found in increased amounts in men who have prostate cancer or other diseases.

In pathology, grading is a measure of the cell appearance in tumors and other neoplasms. Some pathology grading systems apply only to malignant neoplasms (cancer); others apply also to benign neoplasms. The neoplastic grading is a measure of cell anaplasia in the sampled tumor and is based on the resemblance of the tumor to the tissue of origin. Grading in cancer is distinguished from staging, which is a measure of the extent to which the cancer has spread.

The Gleason grading system is used to help evaluate the prognosis of men with prostate cancer using samples from a prostate biopsy. Together with other parameters, it is incorporated into a strategy of prostate cancer staging which predicts prognosis and helps guide therapy. A Gleason score is given to prostate cancer based upon its microscopic appearance. Cancers with a higher Gleason score are more aggressive and have a worse prognosis. Pathological scores range from 2 to 10, with higher numbers indicating greater risks and higher mortality. The system is widely accepted and used for clinical decision making even as it is recognised that certain biomarkers, like ACP1 expression, might yield higher predictive value for future disease course.

Endometrial intraepithelial neoplasia (EIN) is a premalignant lesion of the uterine lining that predisposes to endometrioid endometrial adenocarcinoma. It is composed of a collection of abnormal endometrial cells, arising from the glands that line the uterus, which have a tendency over time to progress to the most common form of uterine cancer—endometrial adenocarcinoma, endometrioid type.

Vulvar cancer is a cancer of the vulva, the outer portion of the female genitals. It most commonly affects the labia majora. Less often, the labia minora, clitoris, or vaginal glands are affected. Symptoms include a lump, itchiness, changes in the skin, or bleeding from the vulva.

Endometrial hyperplasia is a condition of excessive proliferation of the cells of the endometrium, or inner lining of the uterus.

Homeobox protein Nkx-3.1, also known as NKX3-1, NKX3, BAPX2, NKX3A and NKX3.1 is a protein that in humans is encoded by the NKX3-1 gene located on chromosome 8p. NKX3-1 is a prostatic tumor suppressor gene.

Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.

Lobular carcinoma in situ (LCIS) is an incidental microscopic finding with characteristic cellular morphology and multifocal tissue patterns. The condition is a laboratory diagnosis and refers to unusual cells in the lobules of the breast. The lobules and acini of the terminal duct-lobular unit (TDLU), the basic functional unit of the breast, may become distorted and undergo expansion due to the abnormal proliferation of cells comprising the structure. These changes represent a spectrum of atypical epithelial lesions that are broadly referred to as lobular neoplasia (LN).
In urologic pathology, atypical small acinar proliferation, is a collection of small prostatic glands, on prostate biopsy, whose significance is uncertain and cannot be determined to be benign or malignant.
The Bethesda system (TBS), officially called The Bethesda System for Reporting Cervical Cytology, is a system for reporting cervical or vaginal cytologic diagnoses, used for reporting Pap smear results. It was introduced in 1988 and revised in 1991, 2001, and 2014. The name comes from the location of the conference, sponsored by the National Institutes of Health, that established the system.
In pathology, perineural invasion, abbreviated PNI, refers to the invasion of cancer to the space surrounding a nerve. It is common in head and neck cancer, prostate cancer and colorectal cancer.

Fetal adenocarcinoma (FA) of the lung is a rare subtype of pulmonary adenocarcinoma that exhibits tissue architecture and cell characteristics that resemble fetal lung tissue upon microscopic examination. It is currently considered a variant of solid adenocarcinoma with mucin production.
Microglandular hyperplasia (MGH) of the cervix is an epithelial benign abnormality (lesion) associated with gland proliferation. It can terminate in mature squamous metaplasia, and it is suspected reserve cells are involved in this process, perhaps in the form of reserve cell hyperplasia with glandular differentiation.
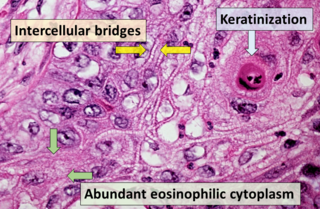
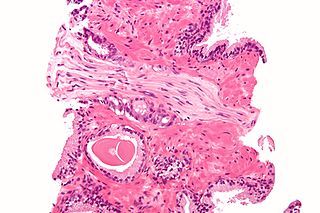
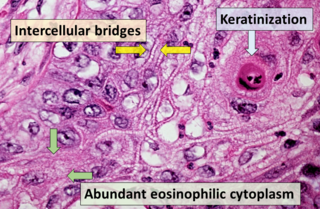
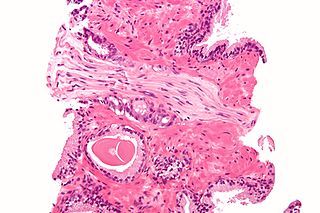
Squamous-cell carcinoma (SCC), also known as epidermoid carcinoma, comprises a number of different types of cancer that begin in squamous cells. These cells form on the surface of the skin, on the lining of hollow organs in the body, and on the lining of the respiratory and digestive tracts.
A histopathologic diagnosis of prostate cancer is the discernment of whether there is a cancer in the prostate, as well as specifying any subdiagnosis of prostate cancer if possible. The histopathologic subdiagnosis of prostate cancer has implications for the possibility and methodology of any subsequent Gleason scoring. The most common histopathological subdiagnosis of prostate cancer is acinar adenocarcinoma, constituting 93% of prostate cancers. The most common form of acinar adenocarcinoma, in turn, is "adenocarcinoma, not otherwise specified", also termed conventional, or usual acinar adenocarcinoma.

The histopathology of colorectal cancer of the adenocarcinoma type involves analysis of tissue taken from a biopsy or surgery. A pathology report contains a description of the microscopical characteristics of the tumor tissue, including both tumor cells and how the tumor invades into healthy tissues and finally if the tumor appears to be completely removed. The most common form of colon cancer is adenocarcinoma, constituting between 95% and 98% of all cases of colorectal cancer. Other, rarer types include lymphoma, adenosquamous and squamous cell carcinoma. Some subtypes have been found to be more aggressive.

Invasive cribriform carcinoma of the breast (ICCB), also termed invasive cribriform carcinoma, is a rare type of breast cancer that accounts for 0.3% to 0.6% of all carcinomas in the breast. It originates in a lactiferous duct as opposed to the lobules that form the alveoli in the breasts' mammary glands. ICCB was first described by Dixon and colleagues in 1983 as a tumor that on microscopic histopathological inspection had a cribriform pattern, i.e. a tissue pattern consisting of numerous "Swiss cheese"-like open spaces and/or sieve-like small holes. The latest edition (2019) of the World Health Organization (2019) termed these lesions invasive cribriform carcinomas indicating that by definition they must have a component that invades out of their ducts of origin into adjacent tissues. In situ ductal cancers that have a cribriform histopathology are regarded as belonging to the group of ductal carcinoma in situ tumors.