Related Research Articles
Algeria is the largest country in Africa and is estimated to have a population of around 46,278,751 people. Algeria has a public health care system, which is accessible and free of charge to all citizens of Algeria. The public health care system is financed by the government of Algeria. Given Algeria's young population, policy favors preventive health care and clinics over hospitals. In keeping with this policy, the government maintains an intensive immunization programme and a policy which allows Algerian citizens health care for Hospitalisations, medicines and outpatient care free to all citizens of Algeria.

Despite the significant progress Yemen has made to expand and improve its health care system over the past decade, the system remains severely underdeveloped. Total expenditures on health care in 2002 constituted 3.7 percent of gross domestic product.

Healthcare in Russia is provided by the state through the Federal Compulsory Medical Insurance Fund, and regulated through the Ministry of Health. The Constitution of the Russian Federation has provided all citizens the right to free healthcare since 1993. In 2008, 621,000 doctors and 1.3 million nurses were employed in Russian healthcare. The number of doctors per 10,000 people was 43.8, but only 12.1 in rural areas. The number of general practitioners as a share of the total number of doctors was 1.26 percent. There are about 9.3 beds per thousand population—nearly double the OECD average.

The major causes of deaths in Finland are cardiovascular diseases, malignant tumors, dementia and Alzheimer's disease, respiratory diseases, alcohol related diseases and accidental poisoning by alcohol. In 2010, the leading causes of death among men aged 15 to 64 were alcohol related deaths, ischaemic heart disease, accident, suicides, lung cancer and cerebrovascular diseases. Among women the leading causes were breast cancer, alcohol related deaths, accidents, suicides, ischaemic heart disease and lung cancer.

Italy's healthcare system is consistently ranked among the best in the world. The Italian healthcare system employs a Beveridge model, and operates on the assumption that health care is a human right that should be provided to everyone regardless of their ability to pay. Life expectancy is the 4th highest among OECD countries and the world's 8th highest according to the WHO. Healthcare spending accounted for 9.7% of GDP in 2020.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).

A landlocked sub-Saharan country, Burkina Faso is among the poorest countries in the world—44 percent of its population lives below the international poverty line of US$1.90 per day —and it ranks 185th out of 188 countries on UNDP's 2016 Human Development Index. Rapid population growth, gender inequality, and low levels of educational attainment contribute to food insecurity and poverty in Burkina Faso. The total population is just over 20 million with the estimated population growth rate is 3.1 percent per year and seven out of 10 Burkinabe are younger than 30. Total health care expenditures were an estimated 5% of GDP. Total expenditure on health per capita is 82 in 2014.

Healthcare in the United States is largely provided by private sector healthcare facilities, and paid for by a combination of public programs, private insurance, and out-of-pocket payments. The U.S. is the only developed country without a system of universal healthcare, and a significant proportion of its population lacks health insurance. The United States spends more on healthcare than any other country, both in absolute terms and as a percentage of GDP; however, this expenditure does not necessarily translate into better overall health outcomes compared to other developed nations. Coverage varies widely across the population, with certain groups, such as the elderly and low-income individuals, receiving more comprehensive care through government programs such as Medicaid and Medicare.
The health status of Namibia has increased steadily since independence, and the government does have focus on health in the country and seeks to make health service upgrades. As a guidance to achieve this goal, the Institute for Health Metrics and Evaluation (IHME) and World Health Organization (WHO) recently published the report "Namibia: State of the Nation's Health: Findings from the Global Burden of Disease." The report backs the fact that Namibia has made steady progress in the last decades when it comes to general health and communicable diseases, but despite this progress, HIV/AIDS still is the major reason for low life expectancy in the country.
Examples of health care systems of the world, sorted by continent, are as follows.
For the period between 2005 and 2010, El Salvador had the third-lowest birth rate in Central America, with 22.8 births per 1,000. However, during the same period, it had the highest death rate in Central America, 5.9 deaths per 1,000. In 2015 life expectancy for men was 67.8 years and 77.0 years for women. Healthy life expectancy was 57 for males and 62 for females in 2003. There was considerable improvement in socioeconomic and health status from 1990 to 2015. On June 22, 2020, the Hospital El Salvador, a permanent hospital conversion of the convention center in San Salvador, was opened to the public; it is Latin America's largest hospital and was built to receive COVID-19 patients.
According to the Constitution of Albania, citizens are entitled to healthcare. The healthcare system in Albania is primarily public. The public system is made up of three tiers: primary care, secondary care, and tertiary care. Primary healthcare covers basic health needs. Secondary healthcare is needed when seeing a specialist after being referred to by a general practitioner. Tertiary healthcare funds are dedicated for highly specialized medical care that is needed over a long duration of time. There are over 400 public clinics that offer both primary and secondary healthcare services, along with over 40 public hospitals that offer tertiary healthcare services.

A new measure of expected human capital calculated for 195 countries from 1990 to 2016 and defined for each birth cohort as the expected years lived from age 20 to 64 years and adjusted for educational attainment, learning or education quality, and functional health status was published by The Lancet in September 2018. Latvia had the twenty-first highest level of expected human capital with 23 health, education, and learning-adjusted expected years lived between age 20 and 64 years.

As of 2019 Lithuanian life expectancy at birth was 76.0 and the infant mortality rate was 2.99 per 1,000 births. This is below the EU and OECD average.
The Human Rights Measurement Initiative finds that Suriname is fulfilling 78.4% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Suriname achieves 94.0% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves only 83.2% of what is expected based on the nation's level of income. Suriname falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 57.9% of what the nation is expected to achieve based on the resources (income) it has available.
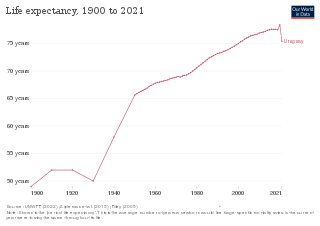
In 2016, the life expectancy in Uruguay was 73 for men and 81 for women.

Brunei's healthcare system is managed by the Brunei Ministry of Health and funded by the General Treasury. It consists of around 15 health centers, ten clinics and 22 maternal facilities, considered to be of reasonable standard. There are also two private hospitals. Cardiovascular disease, cancer, and diabetes are the leading cause of death in the country, with life expectancy around 75 years, a vast improvement from 1961. Brunei's human development index (HCI) improved from 0.81 in 2002 to 0.83 in 2021, expanding at an average annual rate of 0.14%. According to the UN's Human Development Report 2020, the HCI for girls in the country is greater than for boys, though aren't enough statistics in Brunei to break down HCI by socioeconomic classes. Brunei is the second country in Southeast Asia after Singapore to be rated 47th out of 189 nations on the UN HDI 2019 and has maintained its position in the Very High Human Development category. Being a culturally taboo subject, the rate of suicide has not been investigated.
In Nauru, health is challenged by obesity, limited lifespan and childhood health.
Life expectancy in Curaçao was 74.8 years for men and 81.0 years for women in 2016. Infant mortality in 2013 was 11.3 per 1,000 live births.
Life expectancy in Fiji is 66 years for men and 72 years for women. Maternal mortality was 59 per 100 000 live births in 2013.
References
- ↑ "Dominica Life expectancy at birth". Index Mundi. 2017. Retrieved 18 November 2018.
- ↑ "Country Report: Dominica". Pan American Health Organization. 2018. Retrieved 18 November 2018.
- ↑ "Health systems in Dominica". Commonwealth Health online. 2018. Retrieved 18 November 2018.