Related Research Articles

The pupil is a hole located in the center of the iris of the eye that allows light to strike the retina. It appears black because light rays entering the pupil are either absorbed by the tissues inside the eye directly, or absorbed after diffuse reflections within the eye that mostly miss exiting the narrow pupil. The size of the pupil is controlled by the iris, and varies depending on many factors, the most significant being the amount of light in the environment. The term "pupil" was coined by Gerard of Cremona.
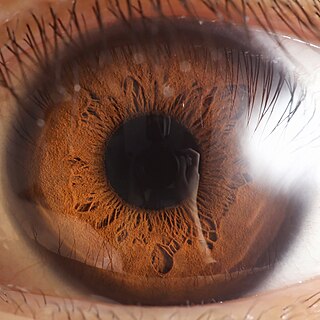
The iris is a thin, annular structure in the eye in most mammals and birds, responsible for controlling the diameter and size of the pupil, and thus the amount of light reaching the retina. In optical terms, the pupil is the eye's aperture, while the iris is the diaphragm. Eye color is defined by the iris.

Mydriasis is the dilation of the pupil, usually having a non-physiological cause, or sometimes a physiological pupillary response. Non-physiological causes of mydriasis include disease, trauma, or the use of certain types of drug. It may also be of unknown cause.

The pupillary light reflex (PLR) or photopupillary reflex is a reflex that controls the diameter of the pupil, in response to the intensity (luminance) of light that falls on the retinal ganglion cells of the retina in the back of the eye, thereby assisting in adaptation of vision to various levels of lightness/darkness. A greater intensity of light causes the pupil to constrict, whereas a lower intensity of light causes the pupil to dilate. Thus, the pupillary light reflex regulates the intensity of light entering the eye. Light shone into one eye will cause both pupils to constrict.

Athetosis is a symptom characterized by slow, involuntary, convoluted, writhing movements of the fingers, hands, toes, and feet and in some cases, arms, legs, neck and tongue. Movements typical of athetosis are sometimes called athetoid movements. Lesions to the brain are most often the direct cause of the symptoms, particularly to the corpus striatum. This symptom does not occur alone and is often accompanied by the symptoms of cerebral palsy, as it is often a result of this physical disability. Treatments for athetosis are not very effective, and in most cases are simply aimed at managing the uncontrollable movement, rather than the cause itself.

The extraocular muscles, or extrinsic ocular muscles, are the seven extrinsic muscles of the eye in humans and other animals. Six of the extraocular muscles, the four recti muscles, and the superior and inferior oblique muscles, control movement of the eye. The other muscle, the levator palpebrae superioris, controls eyelid elevation. The actions of the six muscles responsible for eye movement depend on the position of the eye at the time of muscle contraction.
Oscillopsia is a visual disturbance in which objects in the visual field appear to oscillate. The severity of the effect may range from a mild blurring to rapid and periodic jumping. Oscillopsia is an incapacitating condition experienced by many patients with neurological disorders. It may be the result of ocular instability occurring after the oculomotor system is affected, no longer holding images steady on the retina. A change in the magnitude of the vestibulo-ocular reflex due to vestibular disease can also lead to oscillopsia during rapid head movements. Oscillopsia may also be caused by involuntary eye movements such as nystagmus, or impaired coordination in the visual cortex and is one of the symptoms of superior canal dehiscence syndrome. Those affected may experience dizziness and nausea. Oscillopsia can also be used as a quantitative test to document aminoglycoside toxicity. Permanent oscillopsia can arise from an impairment of the ocular system that serves to maintain ocular stability. Paroxysmal oscillopsia can be due to an abnormal hyperactivity in the peripheral ocular or vestibular system.

The ciliary ganglion is a parasympathetic ganglion located just behind the eye in the posterior orbit. It is 1–2 mm in diameter and in humans contains approximately 2,500 neurons. The ganglion contains postganglionic parasympathetic neurons. These neurons supply the pupillary sphincter muscle, which constricts the pupil, and the ciliary muscle which contracts to make the lens more convex. Both of these muscles are involuntary since they are controlled by the parasympathetic division of the autonomic nervous system.

Adie syndrome, also known as Holmes–Adie syndrome, is a neurological disorder characterized by a tonically dilated pupil that reacts slowly to light but shows a more definite response to accommodation. It is frequently seen in females with absent knee or ankle jerks and impaired sweating.

Parinaud's syndrome is a constellation of neurological signs indicating injury to the dorsal midbrain. More specifically, compression of the vertical gaze center at the rostral interstitial nucleus of medial longitudinal fasciculus (riMLF).
Pupillometer, also spelled pupilometer, is a medical device intended to measure by reflected light the size of the pupil of the eye. In addition to measuring pupil size, current automated pupillometers may also be able to characterize pupillary light reflex. Some instruments for measuring pupillary distance (PD) are often, but incorrectly, referred to as pupilometers.

A relative afferent pupillary defect (RAPD), also known as a Marcus Gunn pupil, is a medical sign observed during the swinging-flashlight test whereupon the patient's pupils excessively dilate when a bright light is swung from the unaffected eye to the affected eye. The affected eye still senses the light and produces pupillary sphincter constriction to some degree, albeit reduced.
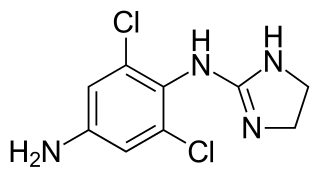
Apraclonidine (INN), also known under the brand name Iopidine, is a sympathomimetic used in glaucoma therapy. It is an α2 adrenergic receptor agonist and a weak α1 adrenergic receptor agonist.

Dilated fundus examination (DFE) is a diagnostic procedure that uses mydriatic eye drops to dilate or enlarge the pupil in order to obtain a better view of the fundus of the eye. Once the pupil is dilated, examiners use ophthalmoscopy to view the eye's interior, which makes it easier to assess the retina, optic nerve head, blood vessels, and other important features. DFE has been found to be a more effective method for evaluating eye health when compared to non-dilated examination, and is the best method of evaluating structures behind the iris. It is frequently performed by ophthalmologists and optometrists as part of an eye examination.
Polycoria is a pathological condition of the eye characterized by more than one pupillary opening in the iris. It may be congenital or result from a disease affecting the iris. It results in decreased function of the iris and pupil, affecting the physical eye and visualization.

Pupillary response is a physiological response that varies the size of the pupil, via the optic and oculomotor cranial nerve.

Nystagmus is a condition of involuntary eye movement. People can be born with it but more commonly acquire it in infancy or later in life. In many cases it may result in reduced or limited vision.

Task-invoked pupillary response is a pupillary response caused by a cognitive load imposed on a human and as a result of the decrease in parasympathetic activity in the peripheral nervous system. It is found to result in a linear increase in pupil dilation as the demand a task places on the working memory increases. Beatty evaluated task-invoked pupillary response in different tasks for short-term memory, language processing, reasoning, perception, sustained attention and selective attention and found that it fulfills Kahneman's three criteria for indicating processing load. That is, it can reflect differences in processing load within a task, between different tasks and between individuals. It is used as an indicator of cognitive load levels in psychophysiology research.
Pupillometry, the measurement of pupil size and reactivity, is a key part of the clinical neurological exam for patients with a wide variety of neurological injuries. It is also used in psychology.
Clinicians routinely check the pupils of critically injured and ill patients to monitor neurological status. However, manual pupil measurements have been shown to be subjective, inaccurate, and not repeatable or consistent. Automated assessment of the pupillary light reflex has emerged as an objective means of measuring pupillary reactivity across a range of neurological diseases, including stroke, traumatic brain injury and edema, tumoral herniation syndromes, and sports or war injuries. Automated pupillometers are used to assess an array of objective pupillary variables including size, constriction velocity, latency, and dilation velocity, which are normalized and standardized to compute an indexed score such as the Neurological Pupil index (NPi).
References
- 1 2 McLaren J. W.; Erie J. C.; Brubaker R. F. (1992). "Computerized analysis of pupillograms in studies of alertness". Investigative Ophthalmology and Visual Science. 33: 671–6.
- 1 2 3 Cassin, B. and Solomon, S. Dictionary of Eye Terminology. Gainesville, Florida: Triad Publishing Company, 1990.
- 1 2 Beatty, J., & Lucero-Wagoner, B. (2000). The pupillary system. In J. T. Cacioppo, L. G. Tassinary & G. G. Bernston (Eds.), The handbook of psychophysiology (2nd ed.) (pp. 142-162). USA: Cambridge University Press.
- ↑ Gerb, Johannes; Brandt, Thomas; Huppert, Doreen (July 2023). "Historical descriptions of nystagmus and abnormal involuntary eye movements in various ancient cultures". Science Progress. 106 (3). doi:10.1177/00368504231191986. ISSN 0036-8504. PMC 10469245 . PMID 37642983.
- ↑ Forensic and State Medicine: Reddy
- 1 2 Denny JC, Arndt FV, Dupont WD, Neilson EG (2008). "Increased hospital mortality in patients with bedside hippus". Am J Med. 121 (3): 239–45. doi:10.1016/j.amjmed.2007.09.014. PMID 18328309.