Otorhinolaryngology is a surgical subspecialty within medicine that deals with the surgical and medical management of conditions of the head and neck. Doctors who specialize in this area are called otorhinolaryngologists, otolaryngologists, head and neck surgeons, or ENT surgeons or physicians. Patients seek treatment from an otorhinolaryngologist for diseases of the ear, nose, throat, base of the skull, head, and neck. These commonly include functional diseases that affect the senses and activities of eating, drinking, speaking, breathing, swallowing, and hearing. In addition, ENT surgery encompasses the surgical management of cancers and benign tumors and reconstruction of the head and neck as well as plastic surgery of the face, scalp, and neck.

Sleep apnea, British English sleep apnoea or sleep apnœa, is a sleep-related breathing disorder in which repetitive pauses in breathing, periods of shallow breathing, or collapse of the upper airway during sleep results in poor ventilation and sleep disruption. Each pause in breathing can last for a few seconds to a few minutes and occurs many times a night. A choking or snorting sound may occur as breathing resumes. Common symptoms include daytime sleepiness, snoring, and non restorative sleep despite adequate sleep time. Because the disorder disrupts normal sleep, those affected may experience sleepiness or feel tired during the day. It is often a chronic condition.

Snoring is the vibration of respiratory structures and the resulting sound due to obstructed air movement during breathing while sleeping. The sound may be soft or loud and unpleasant. Snoring during sleep may be a sign, or first alarm, of obstructive sleep apnea (OSA). Research suggests that snoring is one of the factors of sleep deprivation.

The hypoglossal nerve, also known as the twelfth cranial nerve, cranial nerve XII, or simply CN XII, is a cranial nerve that innervates all the extrinsic and intrinsic muscles of the tongue except for the palatoglossus, which is innervated by the vagus nerve.
Apnea, BrE: apnoea, is the temporary cessation of breathing. During apnea, there is no movement of the muscles of inhalation, and the volume of the lungs initially remains unchanged. Depending on how blocked the airways are, there may or may not be a flow of gas between the lungs and the environment. If there is sufficient flow, gas exchange within the lungs and cellular respiration would not be severely affected. Voluntarily doing this is called holding one's breath. Apnea may first be diagnosed in childhood, and it is recommended to consult an ENT specialist, allergist or sleep physician to discuss symptoms when noticed; malformation and/or malfunctioning of the upper airways may be observed by an orthodontist.

Obesity hypoventilation syndrome (OHS) is a condition in which severely overweight people fail to breathe rapidly or deeply enough, resulting in low oxygen levels and high blood carbon dioxide (CO2) levels. The syndrome is often associated with obstructive sleep apnea (OSA), which causes periods of absent or reduced breathing in sleep, resulting in many partial awakenings during the night and sleepiness during the day. The disease puts strain on the heart, which may lead to heart failure and leg swelling.

Positive airway pressure (PAP) is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for "continuous positive airway pressure", which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco. A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.
Upper airway resistance syndrome (UARS) is a sleep disorder characterized by the narrowing of the airway that can cause disruptions to sleep. The symptoms include unrefreshing sleep, fatigue, sleepiness, chronic insomnia, and difficulty concentrating. UARS can be diagnosed by polysomnograms capable of detecting Respiratory Effort-related Arousals. It can be treated with lifestyle changes, functional orthodontics, surgery, mandibular repositioning devices or CPAP therapy. UARS is considered a variant of sleep apnea, although some scientists and doctors believe it to be a distinct disorder.
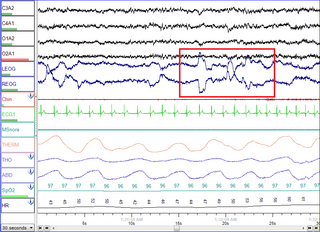
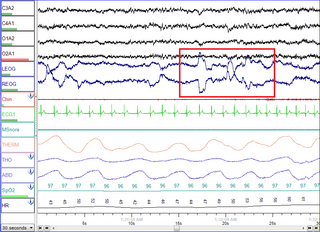
Polysomnography (PSG) is a multi-parameter type of sleep study and a diagnostic tool in sleep medicine. The test result is called a polysomnogram, also abbreviated PSG. The name is derived from Greek and Latin roots: the Greek πολύς, the Latin somnus ("sleep"), and the Greek γράφειν.

Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by recurrent episodes of complete or partial obstruction of the upper airway leading to reduced or absent breathing during sleep. These episodes are termed "apneas" with complete or near-complete cessation of breathing, or "hypopneas" when the reduction in breathing is partial. In either case, a fall in blood oxygen saturation, a disruption in sleep, or both, may result. A high frequency of apneas or hypopneas during sleep may interfere with the quality of sleep, which – in combination with disturbances in blood oxygenation – is thought to contribute to negative consequences to health and quality of life. The terms obstructive sleep apnea syndrome (OSAS) or obstructive sleep apnea–hypopnea syndrome (OSAHS) may be used to refer to OSA when it is associated with symptoms during the daytime.

The genioglossus is one of the paired extrinsic muscles of the tongue. It is a fan-shaped muscle that comprises the bulk of the body of the tongue. It arises from the mental spine of the mandible; it inserts onto the hyoid bone, and the bottom of the tongue. It is innervated by the hypoglossal nerve. The genioglossus is the major muscle responsible for protruding the tongue.
Hypopnea is overly shallow breathing or an abnormally low respiratory rate. Hypopnea is typically defined by a decreased amount of air movement into the lungs and can cause hypoxemia It commonly is due to partial obstruction of the upper airway, but can also have neurological origins in central sleep apnea.

Continuous positive airway pressure (CPAP) is a form of positive airway pressure (PAP) ventilation in which a constant level of pressure greater than atmospheric pressure is continuously applied to the upper respiratory tract of a person. The application of positive pressure may be intended to prevent upper airway collapse, as occurs in obstructive sleep apnea, or to reduce the work of breathing in conditions such as acute decompensated heart failure. CPAP therapy is highly effective for managing obstructive sleep apnea. Compliance and acceptance of use of CPAP therapy can be a limiting factor, with 8% of people stopping use after the first night and 50% within the first year.
Central sleep apnea (CSA) or central sleep apnea syndrome (CSAS) is a sleep-related disorder in which the effort to breathe is diminished or absent, typically for 10 to 30 seconds either intermittently or in cycles, and is usually associated with a reduction in blood oxygen saturation. CSA is usually due to an instability in the body's feedback mechanisms that control respiration. Central sleep apnea can also be an indicator of Arnold–Chiari malformation.
Nasal expiratory positive airway pressure is a treatment for obstructive sleep apnea (OSA) and snoring.
A sleep-related breathing disorder is a sleep disorder in which abnormalities in breathing occur during sleep that may or may not be present while awake. According to the International Classification of Sleep Disorders, sleep-related breathing disorders are classified as follows:
Sleep surgery is a surgery performed to treat sleep disordered breathing. Sleep disordered breathing is a spectrum of disorders that includes snoring, upper airway resistance syndrome, and obstructive sleep apnea. These surgeries are performed by surgeons trained in otolaryngology, oral maxillofacial surgery, and craniofacial surgery.
Hyoid suspension, also known as hyoid myotomy and suspension or hyoid advancement, is a surgical procedure or sleep surgery in which the hyoid bone and its muscle attachments to the tongue and airway are pulled forward with the aim of increasing airway size and improving airway stability in the retrolingual and hypopharyngeal airway. The horseshoe shaped hyoid bone sits directly below the base of tongue with the arms of the bone flanking the airway. Hyoid suspension is typically performed as a treatment for obstructive sleep apnea (OSA). This procedure is frequently performed with a uvulopalatopharyngoplasty (UPPP) which targets sites of obstruction higher in the airway. Typically, a hyoid suspension is considered successful when the patient's apnea-hypopnea index is significantly reduced after surgery.
Oral pressure therapy (OPT) is a treatment for obstructive sleep apnea (OSA) that uses negative pressure in the mouth to shift the soft palate and tongue forward. The negative pressure is created by a bedside console connected by a small tube to a mouthpiece worn inside the mouth during sleep. The device is successful in between a quarter and a third of people.
Transoral robotic surgery (TORS) is a modern surgical technique used to treat tumors of the throat via direct access through the mouth. Transoral robotic sleep apnea (TORSA) surgery utilizes the same approach to open the upper airway of those with obstructive sleep apnea. This technique has gained popularity thanks to its wristed instruments and magnified three-dimensional view, enhancing surgical comfort and precision in remote-access areas.