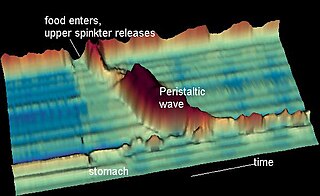
Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver. The digestive system functions to move material through the GI tract via peristalsis, break down that material via digestion, absorb nutrients for use throughout the body, and remove waste from the body via defecation. Physicians who specialize in the medical specialty of gastroenterology are called gastroenterologists or sometimes GI doctors. Some of the most common conditions managed by gastroenterologists include gastroesophageal reflux disease, gastrointestinal bleeding, irritable bowel syndrome, inflammatory bowel disease (IBD) which includes Crohn's disease and ulcerative colitis, peptic ulcer disease, gallbladder and biliary tract disease, hepatitis, pancreatitis, colitis, colon polyps and cancer, nutritional problems, and many more.

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of achalasia exist, but this is neither fully understood, nor agreed upon.

The enteric nervous system (ENS) or intrinsic nervous system is one of the main divisions of the autonomic nervous system (ANS) and consists of a mesh-like system of neurons that governs the function of the gastrointestinal tract. It is capable of acting independently of the sympathetic and parasympathetic nervous systems, although it may be influenced by them. The ENS is nicknamed the "second brain". It is derived from neural crest cells.

The myenteric plexus provides motor innervation to both layers of the muscular layer of the gut, having both parasympathetic and sympathetic input, whereas the submucous plexus provides secretomotor innervation to the mucosa nearest the lumen of the gut.
Functional gastrointestinal disorders (FGID), also known as disorders of gut–brain interaction, include a number of separate idiopathic disorders which affect different parts of the gastrointestinal tract and involve visceral hypersensitivity and motility disturbances.
Postcholecystectomy syndrome (PCS) describes the presence of abdominal symptoms after a cholecystectomy.
The Rome process and Rome criteria are an international effort to create scientific data to help in the diagnosis and treatment of functional gastrointestinal disorders, such as irritable bowel syndrome, functional dyspepsia and rumination syndrome. The Rome diagnostic criteria are set forth by Rome Foundation, a not for profit 501(c)(3) organization based in Raleigh, North Carolina, United States.
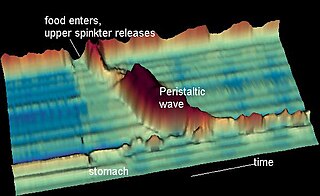
Nutcracker esophagus, jackhammer esophagus, or hypercontractile peristalsis, is a disorder of the movement of the esophagus characterized by contractions in the smooth muscle of the esophagus in a normal sequence but at an excessive amplitude or duration. Nutcracker esophagus is one of several motility disorders of the esophagus, including achalasia and diffuse esophageal spasm. It causes difficulty swallowing, or dysphagia, with both solid and liquid foods, and can cause significant chest pain; it may also be asymptomatic. Nutcracker esophagus can affect people of any age but is more common in the sixth and seventh decades of life.

Paul Enck is Professor of Medical Psychology and was Head of Research at the Department of Psychosomatic Medicine and Psychotherapy, University Hospital Tübingen, Germany until 2014; since then, he holds a part-time research and consultant position at the department. His research interests were and still are psychophysiology and neurogastroenterology. Since his semi-retirement in 2014, he added popular science writing in medicine and history to his activities.
The European Society of Neurogastroenterology & Motility (ESNM) is a professional medical non-profit organization that was founded in 1982. The ESNM has over 3,100 European members, who are involved in the study of neuroscience and the pathophysiology of gastrointestinal function, and more generally in the advancement of neurogastroenterology.
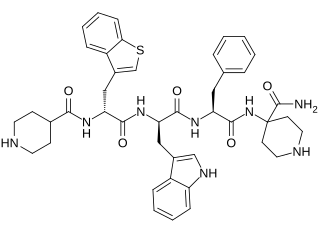
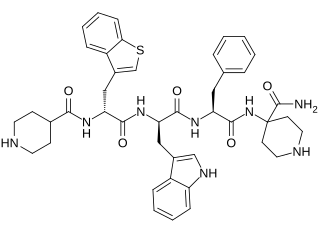
Relamorelin is a synthetic peptide, centrally penetrant, selective agonist of the ghrelin/growth hormone secretagogue receptor (GHSR) which is under development by Allergan pharmaceuticals for the treatment of diabetic gastroparesis, chronic idiopathic constipation, and anorexia nervosa. It is a pentapeptide and an analogue of ghrelin with improved potency and pharmacokinetics. In humans, relamorelin produces increases in plasma growth hormone, prolactin, and cortisol levels, and, like other GHSR agonists, increases appetite. As of June 2015, relamorelin is in phase II clinical trials for diabetic gastroparesis and constipation. The United States Food and Drug Administration (FDA) has granted Fast Track designation to relamorelin for diabetic gastroparesis. The development of the drug is uncertain as the most recent mention of it was in 2019 SEC filing from the drug manufacturer lists the drug's expected launch year as 2024 but not in subsequent filings or press releases.
Hans Gregersen is a Danish bioengineer and scientist. He is regarded as a key figure in the field of gastrointestinal biomechanics and function.
The per-oral endoscopic myotomy, or POEM, is a minimally invasive surgical procedure for the treatment of achalasia wherein the inner circular muscle layer of the lower esophageal sphincter is divided through a submucosal tunnel. This enables food and liquids to pass into the stomach, a process that is impaired in achalasia. The tunnel is created, and the myotomy performed, using a flexible endoscope, meaning the entire procedure can be done without external incisions.

Michel Kahaleh is an American gastroenterologist and an expert in therapeutic endoscopy.

Satish Sanku Chander Rao is the J.Harold Harrison Distinguished University Chair in Gastroenterology at the Medical College of Georgia, Augusta University. He served as the former President of the American Neurogastroenterology and Motility Society and as Chair of the American Gastroenterological Association (AGA) Institute Council, Neurogastroenterology/Motility Section.
Functional Lumen Imaging Probe (FLIP) is a test used to evaluate the function of the esophagus, by measuring the dimensions of the esophageal lumen using impedance planimetry. Typically performed with sedation during upper endoscopy, FLIP is used to evaluate for esophageal motility disorders, such as achalasia, diffuse esophageal spasm, etc.
Prateek SharmaFACG, FACP, FASGE is an Indian American gastroenterologist that specializes in esophageal diseases and endoscopic treatments.

Biliary endoscopic sphincterotomy is a procedure where the sphincter of Oddi and the segment of the common bile duct where it enters the duodenum are cannulated and then cut with a sphincterotome, a device that includes a wire which cuts with an electric current (electrocautery).
Esophagogastric junction outflow obstruction (EGJOO) is an esophageal motility disorder characterized by increased pressure where the esophagus connects to the stomach at the lower esophageal sphincter. EGJOO is diagnosed by esophageal manometry. However, EGJOO has a variety of etiologies; evaluating the cause of obstruction with additional testing, such as upper endoscopy, computed tomography, or endoscopic ultrasound may be necessary. When possible, treatment of EGJOO should be directed at the cause of obstruction. When no cause for obstruction is found, observation alone may be considered if symptoms are minimal. Functional EGJOO with significant or refractor symptoms may be treated with pneumatic dilation, per-oral endoscopic myotomy (POEM), or botulinum toxin injection.

Haruhiro Inoue is a Japanese thoracic surgeon and endoscopist best known for the development of the cap endoscopic mucosal resection technique, and the first per-oral endoscopic myotomy performed in humans. He is a professor at Showa University and Director of the Digestive Disease Centre at Showa University Koto-Toyosu Hospital in Tokyo. He is known for his work in endoscopy and his contribution to the development of endoscopic technologies and procedures.