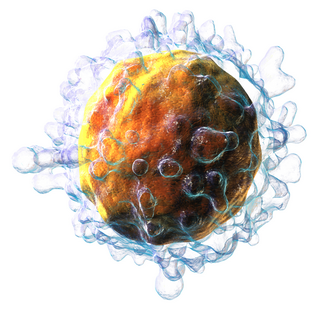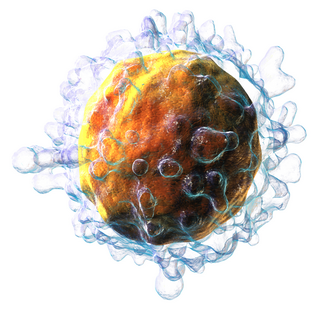
T cells are one of the important types of white blood cells of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell receptor (TCR) on their cell surface.

A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular pathogens (such as viruses or bacteria), or cells that are damaged in other ways.

The T helper cells (Th cells), also known as CD4+ cells or CD4-positive cells, are a type of T cell that play an important role in the adaptive immune system. They aid the activity of other immune cells by releasing cytokines. They are considered essential in B cell antibody class switching, breaking cross-tolerance in dendritic cells, in the activation and growth of cytotoxic T cells, and in maximizing bactericidal activity of phagocytes such as macrophages and neutrophils. CD4+ cells are mature Th cells that express the surface protein CD4. Genetic variation in regulatory elements expressed by CD4+ cells determines susceptibility to a broad class of autoimmune diseases.

Cellular immunity, also known as cell-mediated immunity, is an immune response that does not rely on the production of antibodies. Rather, cell-mediated immunity is the activation of phagocytes, antigen-specific cytotoxic T-lymphocytes, and the release of various cytokines in response to an antigen.
In immunology, central tolerance is the process of eliminating any developing T or B lymphocytes that are autoreactive, i.e. reactive to the body itself. Through elimination of autoreactive lymphocytes, tolerance ensures that the immune system does not attack self peptides. Lymphocyte maturation occurs in primary lymphoid organs such as the bone marrow and the thymus. In mammals, B cells mature in the bone marrow and T cells mature in the thymus.
Gut-associated lymphoid tissue (GALT) is a component of the mucosa-associated lymphoid tissue (MALT) which works in the immune system to protect the body from invasion in the gut.
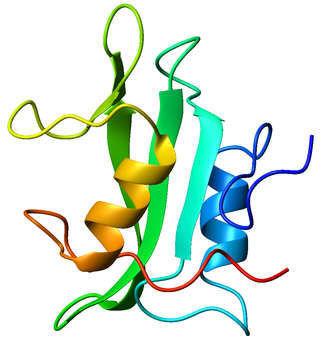
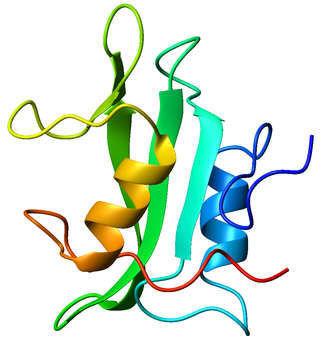
Tyrosin-protein kinase Lck is a 56 kDa protein that is found inside lymphocytes and encoded in the human by the LCK gene. The Lck is a member of Src kinase family (SFK) and is important for the activation of T-cell receptor (TCR) signaling in both naive T cells and effector T cells. The role of Lck is less prominent in the activation or in the maintenance of memory CD8 T cells in comparison to CD4 T cells. In addition, the constitutive activity of the mouse Lck homolog varies among memory T cell subsets. It seems that in mice, in the effector memory T cell (TEM) population, more than 50% of Lck is present in a constitutively active conformation, whereas less than 20% of Lck is present as active form in central memory T cells. These differences are due to differential regulation by SH2 domain–containing phosphatase-1 (Shp-1) and C-terminal Src kinase.
Memory T cells are a subset of T lymphocytes that might have some of the same functions as memory B cells. Their lineage is unclear.
Gamma delta T cells are T cells that have a γδ T-cell receptor (TCR) on their surface. Most T cells are αβ T cells with TCR composed of two glycoprotein chains called α (alpha) and β (beta) TCR chains. In contrast, γδ T cells have a TCR that is made up of one γ (gamma) chain and one δ (delta) chain. This group of T cells is usually less common than αβ T cells. Their highest abundance is in the gut mucosa, within a population of lymphocytes known as intraepithelial lymphocytes (IELs).

Protein tyrosine phosphatase non-receptor type 22 (PTPN22) is a cytoplasmatic protein encoded by gene PTPN22 and a member of PEST family of protein tyrosine phosphatases. This protein is also called "PEST-domain Enriched Phosphatase" ("PEP") or "Lymphoid phosphatase" ("LYP"). The name LYP is used strictly for the human protein encoded by PTPN22, but the name PEP is used only for its mouse homolog. However, both proteins have similar biological functions and show 70% identity in amino acid sequence. PTPN22 functions as a negative regulator of T cell receptor (TCR) signaling, which maintains homeostasis of T cell compartment.

Lymphocyte-activation gene 3, also known as LAG-3, is a protein which in humans is encoded by the LAG3 gene. LAG3, which was discovered in 1990 and was designated CD223 after the Seventh Human Leucocyte Differentiation Antigen Workshop in 2000, is a cell surface molecule with diverse biological effects on T cell function but overall has an immune inhibitory effect. It is an immune checkpoint receptor and as such is the target of various drug development programs by pharmaceutical companies seeking to develop new treatments for cancer and autoimmune disorders. In soluble form it is also being developed as a cancer drug in its own right.

Thymocyte selection-associated high mobility group box protein TOX is a protein that in humans is encoded by the TOX gene. TOX drives T-cell exhaustion and plays a role in innate lymphoid cell development.
The avian immune system is the system of biological structures and cellular processes that protects birds from disease.

Gabrielle T. Belz is an Australian molecular immunologist and viral immunologist. She is a faculty member of the Walter and Eliza Hall Institute of Medical Research, within the Molecular Immunology division. Belz has made important contributions to the understanding of immune system function, especially in relation to the molecular and cellular signalling pathways of immune response to viruses. Her research has focused on understanding the signals that drive the initial development of protective immunity against pathogen infections, such as influenza and herpes viruses. This includes research into how cytotoxic T cells recognise and remove virally-infected cells from the body following infection. Research into the description of the specific factors and response during infection will contribute towards the long-term development of vaccines for infectious disease, and the development of better treatments for autoimmune diseases.

Akiko Iwasaki is a Sterling Professor of Immunobiology and Molecular, Cellular and Developmental Biology at Yale University. She is also a principal investigator at the Howard Hughes Medical Institute. Her research interests include innate immunity, autophagy, inflammasomes, sexually transmitted infections, herpes simplex virus, human papillomavirus, respiratory virus infections, influenza infection, T cell immunity, commensal bacteria, COVID-19, and long COVID.
Immunology & Cell Biology is an academic journal of the Australian and New Zealand Society for Immunology covering basic immunology research. The journal has a focus on cellular immunology, innate and adaptive immunity, immune responses to pathogens, tumour immunology, immunopathology, immunotherapy, immunogenetics and immunological studies in humans and model organisms. The journal was founded in 1924 as the Australian Journal of Experimental Biology and Medical Science, and was converted in 1987 to Immunology and Cell Biology, making it one of the oldest speciality immunology journals in existence. Major historical contributions including publication by Donald Metcalf of the strategy for identifying colony-stimulating factors (CSFs) and the development of the clonal selection theory by Frank Macfarlane Burnet, in a series of more than 90 publications in the 1970s.
Misty Rayna Jenkins is an Australian scientist known for her research into lymphocytes and cancer treatment.

Robyn S. Klein is an American neuroimmunologist as well as the Vice Provost and Associate Dean for Graduate Education at Washington University in St. Louis. Klein is also a professor in the Departments of Medicine, Anatomy & Neurobiology, and Pathology & Immunology. Her research explores the pathogenesis of neuroinflammation in the central nervous system by probing how immune signalling molecules regulate blood brain barrier permeability. Klein is also a fervent advocate for gender equity in STEM, publishing mechanisms to improve gender equity in speakers at conferences, participating nationally on gender equity discussion panels, and through service as the president of the Academic Women’s Network at the Washington University School of Medicine.
Fabienne Mackay is a French Australian research immunologist and institutional leader within the Australian medical research, education and innovation sectors. She is the Director and CEO of the QIMR Berghofer Medical Research Institute since 2020, after being the inaugural Head of the School of Biomedical Sciences at the University of Melbourne during the preceding five years. She is also an Honorary Professor at the Faculties of Medicine of the University of Queensland and the University of Melbourne. Her work has attracted public attention for its contribution to the pathophysiological understanding and treatment of lupus and other autoimmune diseases. Mackay has been notably awarded, achieving international reputation for her widely cited research describing B-cell activating factor (BAFF) and other cytokines of the TNF receptor superfamily, and their roles in B cell physiology, autoimmunity and cancer. She is an elected Fellow of the Australian Academy of Health and Medical Sciences.
Louise E. Purton is an Australian biologist who is Professor of Medicine and head of the Stem Cell Regulation Laboratory at St. Vincent's Institute of Medical Research in Melbourne. Her research considers the stem cells responsible for the production of blood cells and the regulations of haematopoietic diseases. She was awarded the International Society for Experimental Hematology McCulloch & Till Award in 2022. She has experienced profound bilateral hearing loss since the age of three and has been recognised for her work supporting Equity and Diversity, particularly amongst women and people with disability, and is a member of the AAMRI Gender, Equity and Diversity and Inclusion group GEDI.