Related Research Articles

Assisted suicide, also known as assisted dying or medical aid in dying, is suicide undertaken with the aid of another person. The term usually refers to physician-assisted suicide (PAS), which is suicide that is assisted by a physician or other healthcare provider. Once it is determined that the person's situation qualifies under the physician-assisted suicide laws for that place, the physician's assistance is usually limited to writing a prescription for a lethal dose of drugs.

Thanatology is the scientific study of death and the losses brought about as a result. It investigates the mechanisms and forensic aspects of death, such as bodily changes that accompany death and the postmortem period, as well as wider psychological and social aspects related to death. It is primarily an interdisciplinary study offered as a course of study at numerous colleges and universities.
Terminal illness or end-stage disease is a disease that cannot be cured or adequately treated and is reasonably expected to result in the death of the patient. This term is more commonly used for progressive diseases such as cancer or advanced heart disease than for trauma. In popular use, it indicates a disease that will progress until death with near absolute certainty, regardless of treatment. A patient who has such an illness may be referred to as a terminal patient, terminally ill or simply as being terminal. There is no standardized life expectancy for a patient to be considered terminal, although it is generally months or less. Life expectancy for terminal patients is a rough estimate given by the physician based on previous data and does not always reflect true longevity. An illness which is lifelong but not fatal is a chronic condition.

Elisabeth Kübler-Ross was a Swiss-American psychiatrist, a pioneer in near-death studies, and author of the internationally best-selling book, On Death and Dying (1969), where she first discussed her theory of the five stages of grief, also known as the "Kübler-Ross model".

Dame Cicely Mary Strode Saunders was an English nurse, social worker, physician and writer. She is noted for her work in terminal care research and her role in the birth of the hospice movement, emphasising the importance of palliative care in modern medicine, and opposing the legalisation of voluntary euthanasia.
Death education is education about death that focuses on the human and emotional aspects of death. Though it may include teaching on the biological aspects of death, teaching about coping with grief is a primary focus. Death education is formally known as thanatology. Thanatology stems from the Greek word thanatos, meaning death, and ology meaning a science or organized body of knowledge. A specialist in this field is referred to as a thanatologist. Death education refers to the experiences and activities of death that one deals with. Death education also deals with being able to grasp the different processes of dying, talk about the main topics of attitudes and meanings toward death, and the after effects on how to learn to care for people who are affected by the death. The main focus in death education is teaching people how to cope with grief. Many people feel death education is taboo and instead of talking about death and grieving, they hide it away and never bring it up with others. With the right education about death, the less taboo it may become.

Charles Edmund Cullen is an American serial killer who confessed to murdering up to 40 patients during the course of his 16-year career as a nurse in New Jersey. However, in subsequent interviews with police, psychiatrists, and journalists, it became apparent that he had killed many more, whom he could not specifically remember by name, though he could often remember details of their murders. Experts have estimated that Cullen may ultimately be responsible for 400 deaths, which would make him the most prolific serial killer in recorded history.
Therese Schroeder-Sheker is a musician, educator, clinician, and academic dean of the School of Music-Thanatology, which was housed at St. Patrick Hospital in Missoula, Montana from 1992 to 2002.

Florence Wald was an American nurse, former Dean of Yale School of Nursing, and largely credited as "the mother of the American hospice movement". She led the founding of Connecticut Hospice, the first hospice program in the United States. Late in life, Wald became interested in the provision of hospice care within prisons. In 1998, Wald was inducted into the National Women's Hall of Fame.
Rainbow Hospice and Palliative Care, founded in 1981, is one of the oldest and largest non-profit hospice and palliative care providers in Illinois.

Initiative 1000 (I-1000) of 2008 established the U.S. state of Washington's Death with Dignity Act, which legalizes medical aid in dying with certain restrictions. Passage of this initiative made Washington the second U.S. state to permit some terminally ill patients to determine the time of their own death. The effort was headed by former Governor Booth Gardner.

Hospice care in the United States is a type and philosophy of end-of-life care which focuses on the palliation of a terminally ill patient's symptoms. These symptoms can be physical, emotional, spiritual or social in nature. The concept of hospice as a place to treat the incurably ill has been evolving since the 11th century. Hospice care was introduced to the United States in the 1970s in response to the work of Cicely Saunders in the United Kingdom. This part of health care has expanded as people face a variety of issues with terminal illness. In the United States, it is distinguished by extensive use of volunteers and a greater emphasis on the patient's psychological needs in coming to terms with dying.
Hospice care is a type of health care that focuses on the palliation of a terminally ill patient's pain and symptoms and attending to their emotional and spiritual needs at the end of life. Hospice care prioritizes comfort and quality of life by reducing pain and suffering. Hospice care provides an alternative to therapies focused on life-prolonging measures that may be arduous, likely to cause more symptoms, or are not aligned with a person's goals.

Assisted suicide is defined as suicide committed with the aid of another person, sometimes a doctor. "Assisted suicide" has been used to describe what proponents refer to as medical aid in dying in the United States for terminally ill adults who self-administer barbiturates if they feel that they are suffering significantly. The term is often used interchangeably with physician-assisted suicide (PAS), "physician-assisted dying", "physician-assisted death", "assisted death" and "aid in dying".
David Kessler is an author, public speaker, and death and grieving expert. He has published many books, including two co-written with the psychiatrist Elisabeth Kübler-Ross: Life Lessons: Two Experts on Death and Dying Teach Us About the Mysteries of Life and Living, and On Grief & Grieving: Finding the Meaning of Grief Through the Five Stages of Grief. His first book, The Needs of the Dying, received praise from Mother Teresa and Marianne Williamson.
Linda Jane Laubenstein was an American physician and early HIV/AIDS researcher. She was among the first doctors in the United States to recognize the AIDS epidemic of the early 1980s; she co-authored the first article linking AIDS with Kaposi's sarcoma.

Getting On is an American television comedy series based on the British series of the same name, created and written by Mark V. Olsen and Will Scheffer. The series aired on HBO from November 24, 2013, to December 13, 2015, for three seasons each containing six episodes. The show has garnered positive reviews from critics. It stars Laurie Metcalf, Alex Borstein, Niecy Nash, and Mel Rodriguez.
Lucy Finch is a palliative nurse who has worked in several African countries and founded a hospice in Malawi – Ndi Moyo – "the place giving life".
Margaret Ruth McCorkle FAAN, FAPOS is an international leader and award-winning pioneer in oncology nursing. She is currently the Florence Schorske Wald Professor of Nursing at the Yale School of Nursing.
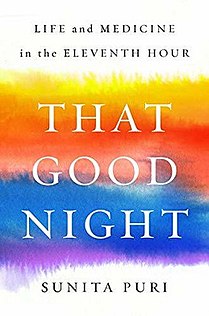
That Good Night: Life and Medicine in the Eleventh Hour is a 2019 memoir written by Dr. Sunita Puri, a palliative care physician who chronicles her experiences with helping terminally-ill patients and their family members make end-of-life decisions. Throughout the span of 13 chapters, Dr. Puri recounts clinical encounters involving both patients and professional colleagues, stories of her upbringing, and personal reflections about the field of palliative medicine. The book was published by Penguin Random House in 2019.
References
- 1 2 3 Ufema, Joy (2007). Insights on Death and Dying. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins. p. x. ISBN 1582559732 – via Google Books.
- 1 2 Harmon, Kate (June 7, 2016). "They gave York AIDS patients a place to die (column)". York Daily Record – York Sunday News. Retrieved September 15, 2016.
The pair continued talking of the old days, with Counsel's partner, Linda, whispering later that she worries that after their retirements the two lost sight of the work they'd done – the lives they changed.
- ↑ "U.S. Public Records Index" . ancestry.com. 1993. Retrieved September 15, 2016.
- 1 2 3 4 "News From Around Here". Tyrone Daily Herald . 113 (247). June 5, 1981. p. 1. Archived from the original on September 15, 2016. Retrieved September 2, 2016– via Newspapers.com
 .
. - ↑ "Obituaries – Counsel". Altoona Mirror. Altoona, Pennsylvania. July 16, 1965.
- 1 2 3 4 5 Bricker, Rebecca (January 19, 1981). "Joy Ufema's Work with the Dying Has Inspired Controversy, a TV Film and Immeasurable Gratitude". People. 15 (2). Archived from the original on September 21, 2016. Retrieved September 2, 2016.
- 1 2 "2004 Distinguished Alumni Award Winners – AASD Foundation/AAHS Alumni Association". aasdfoundation.site-ym.com. Archived from the original on September 20, 2016. Retrieved September 15, 2016.
- 1 2 3 "Hospice director asked to quit". Reading Eagle (273). October 27, 1982. pp. 1 & 8. Retrieved September 2, 2016.
- ↑ "TV-movie deals with dying". Bangor Daily News. January 10, 1981. p. 3ME. Retrieved September 3, 2016.
- 1 2 3 "Joy Ufema will speak at Wilson". The Gettysburg Times. 79 (214). September 11, 1981. p. 7. Retrieved September 2, 2016.
- ↑ Ufema, Joy (1984). Brief Companions. Fawn Grove, Pennsylvania: Mulligan Company. ISBN 0930841018 – via Google books.
- ↑ Dealing with Death and Dying. U.S.: Springhouse Publishing Co. 1991. ISBN 0874343356.
- 1 2 J. Hare, Sharon (December 12, 1992). "York House – A place where final wishes are everything" . Hanover Evening Sun. 161 (89). p. A3. Archived from the original on September 11, 2016. Retrieved September 3, 2016– via Newspaperarchive.com.
- ↑ "AIDS hospice in York shuts down" . Altoona Mirror. Associated Press. November 7, 1996. p. B3. Archived from the original on September 11, 2016. Retrieved September 3, 2016– via Newspaperarchive.com.
- ↑ "Being Fully Present with Joy Ufema". Kanopy. 2007. Archived from the original on September 13, 2016. Retrieved September 3, 2016.
- ↑ Gall Hare, Mary (October 9, 1992). "Assume dying patient knows best, specialist tells hospice workers". The Baltimore Sun. Archived from the original on September 20, 2016. Retrieved September 2, 2016.
- ↑ "Nurse Helps Terminally Ill Prepare To Face Death". Colorado Springs Gazette-Telegraph. Associated Press. February 8, 1978. Archived from the original on September 15, 2016. Retrieved September 2, 2016– via Newspapers.com
 .
.