Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.
Hypereosinophilic syndrome is a disease characterized by a persistently elevated eosinophil count in the blood for at least six months without any recognizable cause, with involvement of either the heart, nervous system, or bone marrow.

Pemphigus is a rare group of blistering autoimmune diseases that affect the skin and mucous membranes. The name is derived from the Greek root pemphix, meaning "blister".
Eosinophilic pneumonia is a disease in which an eosinophil, a type of white blood cell, accumulates in the lungs. These cells cause disruption of the normal air spaces (alveoli) where oxygen is extracted from the atmosphere. Several different kinds of eosinophilic pneumonia exist and can occur in any age group. The most common symptoms include cough, fever, difficulty breathing, and sweating at night. Eosinophilic pneumonia is diagnosed by a combination of characteristic symptoms, findings on a physical examination by a health provider, and the results of blood tests and X-rays. Prognosis is excellent once most eosinophilic pneumonia is recognized and treatment with corticosteroids is begun.

Morphea is a form of scleroderma that mainly involves isolated patches of hardened skin on the face, hands, and feet, or anywhere else on the body, usually with no internal organ involvement. However, in Deep Morphea inflammation and sclerosis can be found in the deep dermis, panniculus, fascia, superficial muscle and bone.

Eosinophilic esophagitis (EoE) is an allergic inflammatory condition of the esophagus that involves eosinophils, a type of white blood cell. In healthy individuals, the esophagus is typically devoid of eosinophils. In EoE, eosinophils migrate to the esophagus in large numbers. When a trigger food is eaten, the eosinophils contribute to tissue damage and inflammation. Symptoms include swallowing difficulty, food impaction, vomiting, and heartburn.

Vernal keratoconjunctivitis is a recurrent, bilateral, and self-limiting type of conjunctivitis having a periodic seasonal incidence.

Prurigo nodularis (PN), also known as nodular prurigo, is a skin disease characterised by pruritic (itchy) nodules which usually appear on the arms or legs. Patients often present with multiple excoriated lesions caused by scratching. PN is also known as Hyde prurigo nodularis, Picker's nodules, atypical nodular form of neurodermatitis circumscripta, lichen corneus obtusus.
Eosinophilic folliculitis is an itchy rash with an unknown cause that is most common among individuals with HIV, though it can occur in HIV-negative individuals where it is known by the eponym Ofuji disease. EF consists of itchy red bumps (papules) centered on hair follicles and typically found on the upper body, sparing the abdomen and legs. The name eosinophilic folliculitis refers to the predominant immune cells associated with the disease (eosinophils) and the involvement of the hair follicles.

Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, painful, inflamed and coin-shaped patches of skin with a scaly and crusty appearance, most often on the scalp, cheeks, and ears. Hair loss may occur if the lesions are on the scalp. The lesions can then develop severe scarring, and the centre areas may appear lighter in color with a rim darker than the normal skin. These lesions can last for years without treatment.
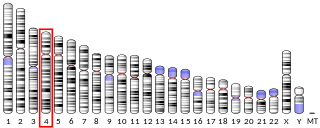
Factor interacting with PAPOLA and CPSF1 is a protein that in humans is encoded by the FIP1L1 gene. A medically important aspect of the FIP1L1 gene is its fusion with other genes to form fusion genes which cause clonal hypereosinophilia and leukemic diseases in humans.
Acute eosinophilic leukemia (AEL) is a rare subtype of acute myeloid leukemia with 50 to 80 percent of eosinophilic cells in the blood and marrow. It can arise de novo or may develop in patients having the chronic form of a hypereosinophilic syndrome. Patients with acute eosinophilic leukemia have a propensity for developing bronchospasm as well as symptoms of the acute coronary syndrome and/or heart failure due to eosinophilic myocarditis and eosinophil-based endomyocardial fibrosis. Hepatomegaly and splenomegaly are more common than in other variants of AML.
Palisaded neutrophilic and granulomatous dermaititis (PNGS) is usually associated with a well-defined connective tissue disease, lupus erythematosus or rheumatoid arthritis most commonly, and often presents with eroded or ulcerated symmetrically distributed umbilicated papules or nodules on the elbows.

Angiolymphoid hyperplasia with eosinophilia usually presents with pink to red-brown, dome-shaped, dermal papules or nodules of the head or neck, especially about the ears and on the scalp.

Eosinophilic cystitis is a rare type of interstitial cystitis first reported in 1960 by Edwin Brown. Eosinophilic cystitis has been linked to a number of etiological factors, including allergies, bladder tumors, trauma to the bladder, parasitic infections, and chemotherapy drugs, though the exact cause of the condition is still unknown. The antigen-antibody response is most likely the cause of eosinophilic cystitis. This results in the generation of different immunoglobulins, which activate eosinophils and start the inflammatory process.
Eosinophilic myocarditis is inflammation in the heart muscle that is caused by the infiltration and destructive activity of a type of white blood cell, the eosinophil. Typically, the disorder is associated with hypereosinophilia, i.e. an eosinophil blood cell count greater than 1,500 per microliter. It is distinguished from non-eosinophilic myocarditis, which is heart inflammation caused by other types of white blood cells, i.e. lymphocytes and monocytes, as well as the respective descendants of these cells, NK cells and macrophages. This distinction is important because the eosinophil-based disorder is due to a particular set of underlying diseases and its preferred treatments differ from those for non-eosinophilic myocarditis.
Clonal hypereosinophilia, also termed primary hypereosinophilia or clonal eosinophilia, is a grouping of hematological disorders all of which are characterized by the development and growth of a pre-malignant or malignant population of eosinophils, a type of white blood cell that occupies the bone marrow, blood, and other tissues. This population consists of a clone of eosinophils, i.e. a group of genetically identical eosinophils derived from a sufficiently mutated ancestor cell.
Lymphocyte-variant hypereosinophilia is a rare disorder in which eosinophilia or hypereosinophilia is caused by an aberrant population of lymphocytes. These aberrant lymphocytes function abnormally by stimulating the proliferation and maturation of bone marrow eosinophil-precursor cells termed colony forming unit-eosinophils or CFU-Eos.

Mosquito bite allergies, also termed hypersensitivity to mosquito bites, are excessive reactions of varying severity to mosquito bites. They are allergic hypersensitivity reactions caused by the non-toxic allergenic proteins contained in the saliva injected by a female mosquito at the time it takes its blood meal, and are not caused by any toxin or pathogen. By general agreement, mosquito bite allergies do not include the ordinary wheal and flare responses to these bites although these reactions are also allergic in nature. Ordinary mosquito bite allergies are nonetheless detailed here because they are the best understood reactions to mosquito bites and provide a basis for describing what is understood about them.