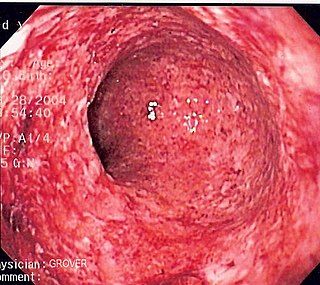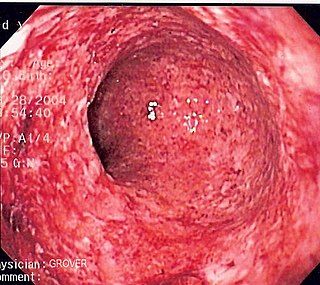
Crohn's disease is a chronic inflammatory bowel disease characterized by recurrent episodes of intestinal inflammation, primarily manifesting as diarrhea and abdominal pain. Unlike ulcerative colitis, inflammation can occur anywhere in the gastrointestinal tract, though it most frequently affects the ileum and colon, involving all layers of the intestinal wall. Symptoms may be non-specific and progress gradually, often delaying diagnosis. About one-third of patients have colonic disease, another third have ileocolic disease, and the remaining third have isolated ileal disease. Systemic symptoms such as chronic fatigue, weight loss, and low-grade fevers are common, along with extraintestinal manifestations affecting organs like the skin and joints. Complications can include bowel obstructions, fistulas, and an increased risk of intestinal cancers.

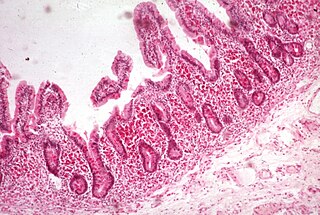
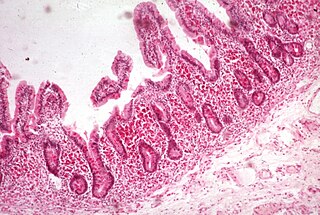
Coeliac disease or celiac disease is a long-term autoimmune disorder, primarily affecting the small intestine, where individuals develop intolerance to gluten, present in foods such as wheat, rye and barley. Classic symptoms include gastrointestinal problems such as chronic diarrhoea, abdominal distention, malabsorption, loss of appetite, and among children failure to grow normally. Non-classic symptoms are more common, especially in people older than two years. There may be mild or absent gastrointestinal symptoms, a wide number of symptoms involving any part of the body, or no obvious symptoms. Coeliac disease was first described in childhood; however, it may develop at any age. It is associated with other autoimmune diseases, such as Type 1 diabetes mellitus and Hashimoto's thyroiditis, among others.

The small intestine or small bowel is an organ in the gastrointestinal tract where most of the absorption of nutrients from food takes place. It lies between the stomach and large intestine, and receives bile and pancreatic juice through the pancreatic duct to aid in digestion. The small intestine is about 5.5 metres long and folds many times to fit in the abdomen. Although it is longer than the large intestine, it is called the small intestine because it is narrower in diameter.

Microvilli are microscopic cellular membrane protrusions that increase the surface area for diffusion and minimize any increase in volume, and are involved in a wide variety of functions, including absorption, secretion, cellular adhesion, and mechanotransduction.
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal (GI) tract. Impairment can be of single or multiple nutrients depending on the abnormality. This may lead to malnutrition and a variety of anaemias.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum; and the accessory organs of digestion, the liver, gallbladder, and pancreas.
Tropical sprue is a malabsorption disease commonly found in tropical regions, marked with abnormal flattening of the villi and inflammation of the lining of the small intestine. It differs significantly from coeliac sprue. It appears to be a more severe form of environmental enteropathy.

Short bowel syndrome is a rare malabsorption disorder caused by a lack of functional small intestine. The primary symptom is diarrhea, which can result in dehydration, malnutrition, and weight loss. Other symptoms may include bloating, heartburn, feeling tired, lactose intolerance, and foul-smelling stool. Complications can include anemia and kidney stones.
Food intolerance is a detrimental reaction, often delayed, to a food, beverage, food additive, or compound found in foods that produces symptoms in one or more body organs and systems, but generally refers to reactions other than food allergy. Food hypersensitivity is used to refer broadly to both food intolerances and food allergies.

Lymphangiectasia, also known as "lymphangiectasis", is a pathologic dilation of lymph vessels. When it occurs in the intestines it is known as intestinal lymphangiectasia, colloquially recognized as Waldmann's disease in cases where there is no secondary cause. The primary defect lies in the inability of the lymphatic system to adequately drain lymph, resulting in its subsequent accumulation and leakage into the intestinal lumen. This condition, first described by Waldmann in 1961, is typically diagnosed in infancy or early childhood. However, it can also manifest in adults, exhibiting a broad spectrum of clinical symptoms.

Protein losing enteropathy (PLE) is a syndrome in which blood proteins are lost excessively via the gastrointestinal (GI) tract. It may be caused by many different underlying diseases that damage the lining of the GI tract (mucosa) or cause blockage of its lymphatic drainage.

Sucrose intolerance or genetic sucrase-isomaltase deficiency (GSID) is the condition in which sucrase-isomaltase, an enzyme needed for proper metabolism of sucrose (sugar) and starch, is not produced or the enzyme produced is either partially functional or non-functional in the small intestine. All GSID patients lack fully functional sucrase, while the isomaltase activity can vary from minimal functionality to almost normal activity. The presence of residual isomaltase activity may explain why some GSID patients are better able to tolerate starch in their diet than others with GSID.
Radiation enteropathy is a syndrome that may develop following abdominal or pelvic radiation therapy for cancer. Many affected people are cancer survivors who had treatment for cervical cancer or prostate cancer. It has also been termed pelvic radiation disease with radiation proctitis being one of its principal features and radiation-induced lumbar plexopathy (RILP) being a rare consequence.

Enteropathy-associated T-cell lymphoma (EATL), previously termed enteropathy-associated T-cell lymphoma, type I and at one time termed enteropathy-type T-cell lymphoma (ETTL), is a complication of coeliac disease in which a malignant T-cell lymphoma develops in areas of the small intestine affected by the disease's intense inflammation. While a relatively rare disease, it is the most common type of primary gastrointestinal T-cell lymphoma.
Chronic diarrheaof infancy, also called toddler's diarrhea, is a common condition typically affecting up to 1.7 billion children between ages 6–30 months worldwide every year, usually resolving by age 4. According to the World Health Organization (WHO), diarrheal disease is the second greatest cause of death in children 5 years and younger. Diarrheal disease takes the lives of 525,000 or more children per year. Diarrhea is characterized as the condition of passing of three or more loose or watery bowel movements within a day sometimes with undigested food visible. Diarrhea is separated into three clinical categories; acute diarrhea may last multiple hours or days, acute bloody diarrhea, also known as dysentery, and finally, chronic or persistent diarrhea which lasts 2–4 weeks or more. There is normal growth with no evidence of malnutrition in the child experiencing persistent diarrhea. In chronic diarrhea there is no evidence of blood in the stool and there is no sign of infection. The condition may be related to irritable bowel syndrome. There are various tests that can be performed to rule out other causes of diarrhea that don't fall under the chronic criteria, including blood test, colonoscopy, and even genetic testing. Most acute or severe cases of diarrhea have treatment guidelines revolving around prescription or non prescription medications based on the cause, but the treatment protocols for chronic diarrhea focus on replenishing the body with lost fluids and electrolytes, because there typically isn't a treatable cause.
Bile acid malabsorption (BAM), known also as bile acid diarrhea, is a cause of several gut-related problems, the main one being chronic diarrhea. It has also been called bile acid-induced diarrhea, cholerheic or choleretic enteropathy, bile salt diarrhea or bile salt malabsorption. It can result from malabsorption secondary to gastrointestinal disease, or be a primary disorder, associated with excessive bile acid production. Treatment with bile acid sequestrants is often effective. Depending on the severity of symptoms, it may be recognised as a disability in the United Kingdom under the Equality Act 2010.
Congenital tufting enteropathy is an inherited disorder of the small intestine that presents with intractable diarrhea in young children.

Autoimmune enteropathy is a rare autoimmune disorder characterized by weight loss from malabsorption, severe and protracted diarrhea, and autoimmune damage to the intestinal mucosa. Autoimmune enteropathy typically occurs in infants and younger children however, adult cases have been reported in literature. Autoimmune enteropathy was first described by Walker-Smith et al. in 1982.
Serum-derived bovine immunoglobulin/protein isolate (SBI) is a medical food product derived from bovine serum obtained from adult cows in the United States. It is sold under the name EnteraGam.
Monomorphic epitheliotropic intestinal T cell lymphoma (MEITL) is an extremely rare peripheral T-cell lymphoma that involves the malignant proliferation of a type of lymphocyte, the T cell, in the gastrointestinal tract. Over time, these T cells commonly spread throughout the mucosal lining of a portion of the GI tract, lead to GI tract nodules and ulcerations, and cause symptoms such as abdominal pain, weight loss, diarrhea, obstruction, bleeding, and/or perforation.