Antimicrobial resistance occurs when microbes evolve mechanisms that protect them from antimicrobials, which are drugs used to treat infections. This resistance affects all classes of microbes, including bacteria, viruses, protozoa, and fungi. Together, these adaptations fall under the AMR umbrella, posing significant challenges to healthcare worldwide. Misuse and improper management of antimicrobials are primary drivers of this resistance, though it can also occur naturally through genetic mutations and the spread of resistant genes.

Beta-lactamases (β-lactamases) are enzymes produced by bacteria that provide multi-resistance to beta-lactam antibiotics such as penicillins, cephalosporins, cephamycins, monobactams and carbapenems (ertapenem), although carbapenems are relatively resistant to beta-lactamase. Beta-lactamase provides antibiotic resistance by breaking the antibiotics' structure. These antibiotics all have a common element in their molecular structure: a four-atom ring known as a beta-lactam (β-lactam) ring. Through hydrolysis, the enzyme lactamase breaks the β-lactam ring open, deactivating the molecule's antibacterial properties.
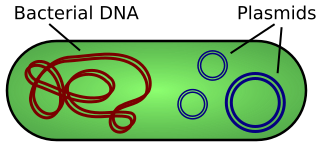
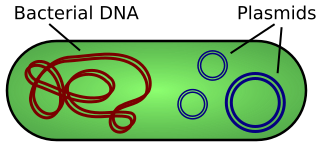
A plasmid is a small, extrachromosomal DNA molecule within a cell that is physically separated from chromosomal DNA and can replicate independently. They are most commonly found as small circular, double-stranded DNA molecules in bacteria; however, plasmids are sometimes present in archaea and eukaryotic organisms. Plasmids often carry useful genes, such as antibiotic resistance and virulence. While chromosomes are large and contain all the essential genetic information for living under normal conditions, plasmids are usually very small and contain additional genes for special circumstances.

Salmonella is a genus of rod-shaped, (bacillus) gram-negative bacteria of the family Enterobacteriaceae. The two known species of Salmonella are Salmonella enterica and Salmonella bongori. S. enterica is the type species and is further divided into six subspecies that include over 2,650 serotypes. Salmonella was named after Daniel Elmer Salmon (1850–1914), an American veterinary surgeon.

Methicillin-resistant Staphylococcus aureus (MRSA) is a group of gram-positive bacteria that are genetically distinct from other strains of Staphylococcus aureus. MRSA is responsible for several difficult-to-treat infections in humans. It caused more than 100,000 deaths worldwide attributable to antimicrobial resistance in 2019.

Klebsiella pneumoniae is a Gram-negative, non-motile, encapsulated, lactose-fermenting, facultative anaerobic, rod-shaped bacterium. It appears as a mucoid lactose fermenter on MacConkey agar.

Vancomycin-resistant Staphylococcus aureus (VRSA) are strains of Staphylococcus aureus that have acquired resistance to the glycopeptide antibiotic vancomycin. Bacteria can acquire resistance genes either by random mutation or through the transfer of DNA from one bacterium to another. Resistance genes interfere with the normal antibiotic function and allow bacteria to grow in the presence of the antibiotic. Resistance in VRSA is conferred by the plasmid-mediated vanA gene and operon. Although VRSA infections are uncommon, VRSA is often resistant to other types of antibiotics and a potential threat to public health because treatment options are limited. VRSA is resistant to many of the standard drugs used to treat S. aureus infections. Furthermore, resistance can be transferred from one bacterium to another.
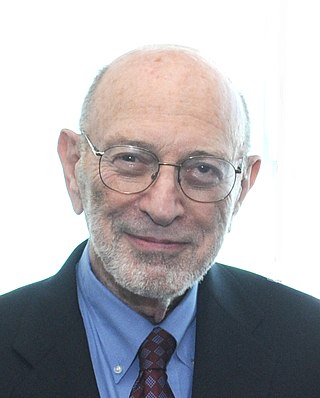
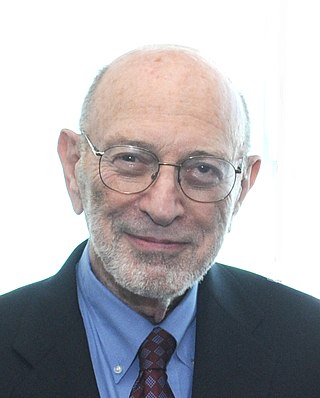
Stanley Norman Cohen is an American geneticist and the Kwoh-Ting Li Professor in the Stanford University School of Medicine. Stanley Cohen and Herbert Boyer were the first scientists to transplant genes from one living organism to another, a fundamental discovery for genetical engineering. Thousands of products have been developed on the basis of their work, including human growth hormone and hepatitis B vaccine. According to immunologist Hugh McDevitt, "Cohen's DNA cloning technology has helped biologists in virtually every field". Without it, "the face of biomedicine and biotechnology would look totally different." Boyer cofounded Genentech in 1976 based on their work together, but Cohen was a consultant for Cetus Corporation and declined to join. In 2022, Cohen was found guilty of having committed fraud in misleading investors into a biotechnology company he founded in 2016, and paid $29 million in damages.
Multiple drug resistance (MDR), multidrug resistance or multiresistance is antimicrobial resistance shown by a species of microorganism to at least one antimicrobial drug in three or more antimicrobial categories. Antimicrobial categories are classifications of antimicrobial agents based on their mode of action and specific to target organisms. The MDR types most threatening to public health are MDR bacteria that resist multiple antibiotics; other types include MDR viruses, parasites.

Stanley "Stan" Falkow was an American microbiologist and a professor of microbiology at Georgetown University, University of Washington, and Stanford University School of Medicine. Falkow is known as the father of the field of molecular microbial pathogenesis. He formulated molecular Koch's postulates, which have guided the study of the microbial determinants of infectious diseases since the late 1980s. Falkow spent over 50 years uncovering molecular mechanisms of how bacteria cause disease and how to disarm them. Falkow also was one of the first scientists to investigate antimicrobial resistance, and presented his research extensively to scientific, government, and lay audiences explaining the spread of resistance from one organism to another, now known as horizontal gene transfer, and the implications of this phenomenon on our ability to combat infections in the future.

Vancomycin-resistant Enterococcus, or vancomycin-resistant enterococci (VRE), are bacterial strains of the genus Enterococcus that are resistant to the antibiotic vancomycin.

Salmonella enterica subsp. enterica is a subspecies of Salmonella enterica, the rod-shaped, flagellated, aerobic, Gram-negative bacterium. Many of the pathogenic serovars of the S. enterica species are in this subspecies, including that responsible for typhoid.
Mary Barber was a British pathologist and bacteriologist who studied antibiotic resistance in bacteria. She was one of the pioneers in this field, documenting the phenomenon of penicillin resistance early on.
Carbapenem-resistant Enterobacteriaceae (CRE) or carbapenemase-producing Enterobacteriaceae (CPE) are gram-negative bacteria that are resistant to the carbapenem class of antibiotics, considered the drugs of last resort for such infections. They are resistant because they produce an enzyme called a carbapenemase that disables the drug molecule. The resistance can vary from moderate to severe. Enterobacteriaceae are common commensals and infectious agents. Experts fear CRE as the new "superbug". The bacteria can kill up to half of patients who get bloodstream infections. Tom Frieden, former head of the Centers for Disease Control and Prevention has referred to CRE as "nightmare bacteria". Examples of enzymes found in certain types of CRE are KPC and NDM. KPC and NDM are enzymes that break down carbapenems and make them ineffective. Both of these enzymes, as well as the enzyme VIM have also been reported in Pseudomonas.
Ruth Milne Hall is an Australian microbiologist whose research on mobile genetic elements in bacteria has provided deep insight into the transfer and evolution of antibiotic resistance in bacteria.

The mobilized colistin resistance (mcr) gene confers plasmid-mediated resistance to colistin, one of a number of last-resort antibiotics for treating Gram-negative infections. mcr-1, the original variant, is capable of horizontal transfer between different strains of a bacterial species. After discovery in November 2015 in E. coli from a pig in China it has been found in Escherichia coli, Salmonella enterica, Klebsiella pneumoniae, Enterobacter aerogenes, and Enterobacter cloacae. As of 2017, it has been detected in more than 30 countries on 5 continents in less than a year.

The 2018 American salmonella outbreak was an American foodborne disaster that started in Iowa, spreading to 7 other states, sickening as many as 265 people, killing one, with 94 hospitalized. Ready-to-eat chicken salad was produced by Iowa-based Triple T Specialty Meats Inc. between January 2 and February 7 for distribution in Fareway grocery stores. Salad was sold in containers of various weights at Fareway stores deli from January 4 to February 9. Total of approximately 20 630 pounds of chicken were deemed contaminated with Salmonella Typhimurium at the time of recall on February 21.

In 2000, typhoid fever caused an estimated 21.7 million illnesses and 217,000 deaths. It occurs most often in children and young adults between 5 and 19 years old. In 2013, it resulted in about 161,000 deaths – down from 181,000 in 1990. Infants, children, and adolescents in south-central and Southeast Asia experience the greatest burden of illness. Outbreaks of typhoid fever are also frequently reported from sub-Saharan Africa and countries in Southeast Asia. In the United States, about 400 cases occur each year, and 75% of these are acquired while traveling internationally.

Karen M. Frank is an American clinical pathologist and microbiologist researching the pathogenesis of Staphylococcus aureus pneumonia and resistant gram-negative bacteria. She is a senior clinician, principal investigator, and chief of laboratory medicine at the National Institutes of Health Clinical Center.