Related Research Articles

The Department of Health and Social Care (DHSC) is a department of His Majesty's Government responsible for government policy on health and adult social care matters in England, along with a few elements of the same matters which are not otherwise devolved to the Scottish Government, Welsh Government or Northern Ireland Executive. It oversees the English National Health Service (NHS). The department is led by the Secretary of State for Health and Social Care with three ministers of state and three parliamentary under-secretaries of state.
NHS Direct was the health advice and information service provided by the National Health Service (NHS), established in March 1998. The nurse-led telephone information service provided residents and visitors in England with healthcare advice 24 hours a day, every day of the year through telephone contact on the national non-geographic 0845 46 47 number. The programme also provided a web based symptom checkers on the NHS Direct website and via mobile, both as apps for iPhone and Android smart phones and a mobile website.

Northwick Park Hospital (NWPH) is a major National Health Service hospital situated in the town of Harrow, North West London, managed by the London North West University Healthcare NHS Trust. It is located off Watford Road in the London Borough of Brent; closely bordering the London Borough of Harrow.
Clinical governance is a systematic approach to maintaining and improving the quality of patient care within the National Health Service (NHS) and private sector health care. Clinical governance became important in health care after the Bristol heart scandal in 1995, during which an anaesthetist, Dr Stephen Bolsin, exposed the high mortality rate for paediatric cardiac surgery at the Bristol Royal Infirmary. It was originally elaborated within the United Kingdom National Health Service (NHS), and its most widely cited formal definition describes it as:
A framework through which NHS organisations are accountable for continually improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish.
Clinical audit is a process that has been defined as a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change
The Healthcare Commission was a non-departmental public body sponsored by the Department of Health of the United Kingdom. It was set up to promote and drive improvement in the quality of health care and public health in England and Wales. It aimed to achieve this by becoming an authoritative and trusted source of information and by ensuring that this information is used to drive improvement. The Commission was abolished on 31 March 2009 and its responsibilities in England broadly subsumed by the Care Quality Commission.
Professor Sir Bruce Edward Keogh, KBE, FMedSci, FRCS, FRCP is a Rhodesian-born British surgeon who specialises in cardiac surgery. He was medical director of the National Health Service in England from 2007 and national medical director of the NHS Commissioning Board from 2013 until his retirement early in 2018. He is chair of Birmingham Women's and Children's NHS Foundation Trust.

NHS Scotland, sometimes styled NHSScotland, is the publicly funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, supported by seven special non-geographic health boards, and Public Health Scotland.
A Patient Safety Organization (PSO) is a group, institution, or association that improves medical care by reducing medical errors. Common functions of patient safety organizations are data collection, analysis, reporting, education, funding, and advocacy. A PSO differs from a Federally designed Patient Safety Organization (PSO), which provides health care providers in the U.S. privilege and confidentiality protections for efforts to improve patient safety and the quality of patient care delivery

The East of England Ambulance Service NHS Trust (EEAST) is an NHS trust responsible for providing National Health Service (NHS) ambulance services in the counties of Bedfordshire, Cambridgeshire, Essex, Hertfordshire, Norfolk and Suffolk, in the East of England region. These consist of approximately 6.2 million people across an area of 7,500 square miles (19,000 km2).

Emergency medical services in the United Kingdom provide emergency care to people with acute illness or injury and are predominantly provided free at the point of use by the four National Health Services (NHS) of England, Scotland, Wales, and Northern Ireland. Emergency care including ambulance and emergency department treatment is only free to UK residents and a charge may be made to those not entitled to free NHS care.
Healthcare in England is mainly provided by the National Health Service (NHS), a public body that provides healthcare to all permanent residents in England, that is free at the point of use. The body is one of four forming the UK National Health Service as health is a devolved matter; there are differences with the provisions for healthcare elsewhere in the United Kingdom, and in England it is overseen by NHS England. Though the public system dominates healthcare provision in England, private health care and a wide variety of alternative and complementary treatments are available for those willing and able to pay.
Healthcare Improvement Scotland (HIS) is the national healthcare improvement organisation for Scotland. It is a public body which is part of the Scottish National Health Service, created in April 2011.
Health care quality is a level of value provided by any health care resource, as determined by some measurement. As with quality in other fields, it is an assessment of whether something is good enough and whether it is suitable for its purpose. The goal of health care is to provide medical resources of high quality to all who need them; that is, to ensure good quality of life, cure illnesses when possible, to extend life expectancy, and so on. Researchers use a variety of quality measures to attempt to determine health care quality, including counts of a therapy's reduction or lessening of diseases identified by medical diagnosis, a decrease in the number of risk factors which people have following preventive care, or a survey of health indicators in a population who are accessing certain kinds of care.
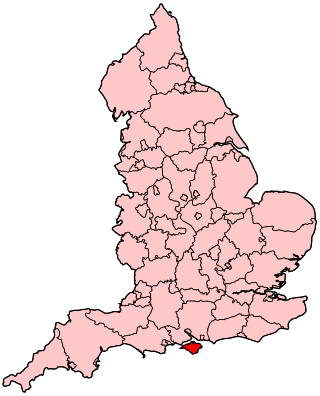
The Isle of Wight NHS Trust is an NHS trust which provides physical health, mental health and ambulance services for the Isle of Wight. The trust is unique in being the only integrated acute, community, mental health and ambulance health care provider in England. It runs St Mary's Hospital and the Isle of Wight Ambulance Service.
Shrewsbury and Telford Hospital NHS Trust is the main provider of hospital services for Shropshire, Telford and Wrekin and North Powys. It runs the Royal Shrewsbury Hospital, the Princess Royal Hospital in Telford, Oswestry Maternity Unit, and Wrekin Community Clinic, Euston House, Telford, in Shropshire, England. It is one of a small number of English NHS Trusts which takes patients from over the border in Wales.
Practitioner Performance Advice, formerly the National Clinical Assessment Service (NCAS), is an organisation that works towards the resolution of concerns about professional practice in healthcare settings across the United Kingdom. By providing their expertise to assist healthcare organisations and individuals resolve concerns, the work of this organisation contributes to improved patient safety.
The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) is a registered charity based in London. Dr Marisa Mason is the Chief Executive and Ian Martin is the Chair of the Trustees. The organisation started from a pilot study of mortality associated with anaesthesia in five regions in England, Wales and Scotland published in 1982. A joint venture was established between surgery and anaesthesia named the Confidential Enquiry into Perioperative Deaths. It became the National Confidential Enquiry into Perioperative Deaths (NCEPOD) in 1988 and published its first report in 1990. It now covers all specialities and covers all outcomes as well as deaths.
The Healthcare Safety Investigation Branch (HSIB) is the independent national investigator for patient safety in England. HSIB was formed in April 2017 and investigates serious patient safety risks that span the healthcare system, operating independently of other regulatory agencies. It aims to produce rigorous, non-punitive, and systematic investigations and to develop system-wide recommendations for learning and improvement and to be separate from systems that seek to allocate blame, liability, or punishment.
A significant event audit (SEA), also known as significant event analysis, is a method of formally assessing significant events, particularly in primary care in the UK, with a view to improving patient care and services. To be effective, the SEA frequently seeks contributions from all members of the healthcare team and involves a subsequent discussion to answer why the occurrence happened and what lessons can be learned. Events triggering a SEA can be diverse, include both adverse and critical events, as well as good practice. It is most frequently required for appraisal, revalidation and continuing professional development.
References
- ↑ "About the Patient Safety division". National Patient Safety Agency. Retrieved 10 August 2014.
- ↑ "NHS aims to improve patient safety". BBC News. 17 April 2001. Retrieved 10 August 2014.
- ↑ "National Clinical Assessment Service to be hosted by NICE". National Clinical Assessment Service. 19 April 2012. Retrieved 10 August 2014.
- ↑ "A Safer Place for Patients: Learning to improve patient safety" (PDF). National Audit Office. 3 November 2005. p. 5. Retrieved 10 August 2014.
- ↑ "Transfer of Patient Safety function to the NHS Commissioning Board Special Health Authority". National Patient Safety Agency. 31 May 2012. Retrieved 10 August 2014.
- ↑ England, NHS. "NHS England » Patient safety". www.england.nhs.uk. Retrieved 16 March 2018.
- ↑ "What we do". NHS Improvement. 1 April 2019. Retrieved 18 May 2020.