The ME Association is a UK health charitable organization that provides information, advocacy, and services to persons and families affected by ME/CFS, and raises funds for research into ME/CFS. It has been reported to be one of the two largest UK charities for ME/CFS.
Rintatolimod, sold under the tradename Ampligen, is a medication intended for treatment of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). There is some evidence it may improve some ME/CFS symptoms.

Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) has a long history with an evolution in medical understanding, diagnoses and social perceptions.
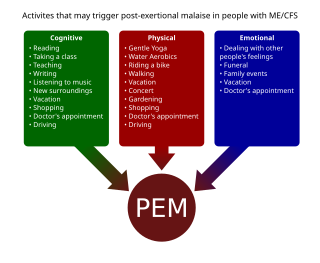
Management of ME/CFS focusses on symptoms management, as no treatments that address the root cause of the illness are available. Pacing, or regulating one's activities to avoid triggering worse symptoms, is the most common management strategy for post-exertional malaise. Clinical management varies widely, with many patients receiving combinations of therapies.

Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is an illness with a history of controversy. Although it is classified as an organic disease, it was historically assumed to be psychosocial, and a minority of medical professionals still hold this view. The pathophysiology of ME/CFS remains unclear, there exists many competing diagnostic criteria, and some proposed treatments are controversial. There is a lack of awareness about the condition, which has led to substantiated accusations of patient neglect and harm.

Clinical descriptions of ME/CFS vary. Different groups have produced sets of diagnostic criteria that share many similarities. The biggest differences between criteria are whether post-exertional malaise (PEM) is required, and the number of symptoms needed.
The Lightning Process (LP) is a three-day personal training programme developed and trademarked by British osteopath Phil Parker. It makes unsubstantiated claims to be beneficial for various conditions, including ME/CFS, depression and chronic pain.
Graded exercise therapy (GET) is a programme of physical activity that starts very slowly and gradually increases over time, intended as a treatment for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Most public health bodies, including the CDC and NICE, consider it ineffective, and its safety is disputed. However, GET still enjoys support among a minority of clinicians and organizations.
David Sheffield Bell is an American physician who has done extensive research on the clinical aspects of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). He has also conducted evaluations and research in pediatric ME/CFS and written numerous articles about the condition.
Daniel Peterson is an American physician in private practice in the state of Nevada, and has been described as a "pioneer" in the treatment of chronic fatigue syndrome (CFS). He graduated from the University of Rochester School of Medicine, Rochester, New York, in 1976 and was an intern and resident at the University of Utah Medical Center from 1976 to 1979. In 1979, he became a diplomate of the American Board of Internal Medicine. He is president of Sierra Internal Medicine of Incline Village, established in 1981.
The Chronic Fatigue Syndrome Advisory Committee (CFSAC) was formed in response to the use of funds by the United States Centers for Disease Control and Prevention in the study of chronic fatigue syndrome (CFS). The CFSAC was charted under the Public Health Service Act of the US and funded by the United States Department of Health and Human Services (HHS). The CFSAC advises the Secretary of Health and Human Services on issues related to its mandate, including issues related to access and care for individuals with CFS, research, public health, clinical care and education regarding CFS. In November, 2008, support for CFSAC activities was changed to the Office on Women's Health, a division of the Office of Public Health and Science. It held it first meeting in 2003.
Dr. José Gilberto Montoya is a prominent researcher known for his contributions to the field of infectious diseases, particularly in the area of chronic fatigue syndrome (CFS) and the role of infectious agents in its development. His research has shed light on the potential involvement of pathogens and immune dysregulation in the pathophysiology of CFS. He was a Professor of Medicine in Infectious Disease at the Stanford University School of Medicine, where he led Stanford's Initiative on Chronic Fatigue Syndrome. He has worked on a wide variety of projects, including research focused on the efficacy of new smallpox vaccines. Additionally, he was the founder and co-director of the Immunocompromised Host Service and works at the Positive Care Clinic at Stanford. He is originally from Cali, Colombia.
Whittemore Peterson Institute (WPI) is a 501(c)(3) nonprofit medical research institute dedicated to scientific discovery surrounding complex neuroimmune diseases including chronic fatigue syndrome (CFS) and other similarly presenting illnesses. Founded in 2005, it is currently located within the Center for Molecular Medicine at the University of Nevada, Reno. It was founded in 2005.

Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a serious long-term illness. People with ME/CFS experience a profound fatigue that does not go away with rest, sleep issues and problems with memory or concentration. They are able to do much less than before they became ill. Further common symptoms include dizziness, nausea and pain. The hallmark symptom is a worsening of the illness hours to days after minor physical or mental activity. This "crash" can last less than a day to several months.
Ronald Wayne "Ron" Davis is professor of biochemistry and genetics, and director of the Stanford Genome Technology Center at Stanford University. Davis is a researcher in biotechnology and molecular genetics, particularly active in human and yeast genomics and the development of new technologies in genomics, with over 30 biotechnology patents. In 2013, it was said of Davis that "A substantial number of the major genetic advances of the past 20 years can be traced back to Davis in some way." Since his son fell severely ill with myalgic encephalomyelitis/chronic fatigue syndrome Davis has focused his research efforts into the illness.
Jennifer Brea is an American documentary filmmaker and activist. Her debut feature, Unrest, premiered at the 2017 Sundance Film Festival and received the US Documentary Special Jury Award For Editing. Brea also co-created a virtual reality film which premiered at Tribeca Film Festival.
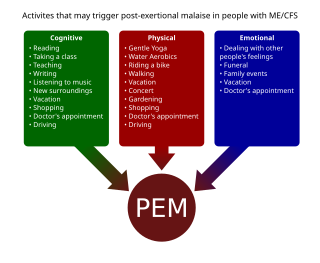
Post-exertional malaise (PEM), sometimes referred to as post-exertional symptom exacerbation (PESE) or post-exertional neuroimmune exhaustion (PENE), is a worsening of symptoms that occurs after minimal exertion. It is the hallmark symptom of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and common in long COVID and fibromyalgia. PEM is often severe enough to be disabling, and is triggered by ordinary activities that healthy people tolerate. Typically, it begins 12–48 hours after the activity that triggers it, and lasts for days, but this is highly variable and may persist much longer. Management of PEM is symptom-based, and patients are recommended to pace their activities to avoid triggering PEM.
Idiopathic chronic fatigue (ICF) or chronic idiopathic fatigue or insufficient/idiopathic fatigue is a term used for cases of unexplained fatigue that have lasted at least six consecutive months and which do not meet the criteria for Myalgic Encephalomyelitis/chronic fatigue syndrome. Such fatigue is widely understood to have a profound effect on the lives of patients who experience it.

DecodeME is an ongoing genome-wide association study searching for genetic risk factors for ME/CFS. With a planned recruitment of 25,000 patients, it is expected to be the largest such study to date. Recruitment closed on 15 November 2023 and results are expected in 2024.
Carmen Scheibenbogen is a German immunologist who is the acting director of the Institute for Medical Immunology of the Charité university hospital in Berlin. She specialises in hematology, oncology and immunology. She leads the Outpatient Clinic for Immunodeficiency and the Fatigue Centre at the Charité hospital. She is one of the few doctors specialised in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in Germany, and also researches long COVID.