A convulsion is a medical condition where the body muscles contract and relax rapidly and repeatedly, resulting in uncontrolled shaking. Because epileptic seizures typically include convulsions, the term convulsion is often used as a synonym for seizure. However, not all epileptic seizures result in convulsions, and not all convulsions are caused by epileptic seizures. Non-epileptic convulsions have no relation with epilepsy, and are caused by non-epileptic seizures.
Advanced Sleep Phase Disorder (ASPD), also known as the advanced sleep-phase type (ASPT) of circadian rhythm sleep disorder, is a condition that is characterized by a recurrent pattern of early evening sleepiness and very early morning awakening. This sleep phase advancement can interfere with daily social and work schedules, and results in shortened sleep duration and excessive daytime sleepiness. The timing of sleep and melatonin levels are regulated by the body's central circadian clock, which is located in the suprachiasmatic nucleus in the hypothalamus.
Tardive dyskinesia (TD) is a disorder that results in involuntary repetitive body movements, which may include grimacing, sticking out the tongue or smacking the lips. Additionally, there may be chorea or slow writhing movements. In about 20% of people with TD, the disorder interferes with daily functioning. If TD is present in the setting of a long-term drug therapy, reversibility can be determined primarily by severity of symptoms and how long symptoms have been present before the long-term drug has been stopped.

Primary familial brain calcification (PFBC), also known as familial idiopathic basal ganglia calcification (FIBGC) and Fahr's disease, is a rare, genetically dominant or recessive, inherited neurological disorder characterized by abnormal deposits of calcium in areas of the brain that control movement. Through the use of CT scans, calcifications are seen primarily in the basal ganglia and in other areas such as the cerebral cortex.
Neuroacanthocytosis is a label applied to several genetic neurological conditions in which the blood contains misshapen, spiculated red blood cells called acanthocytes.
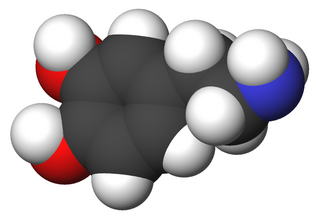
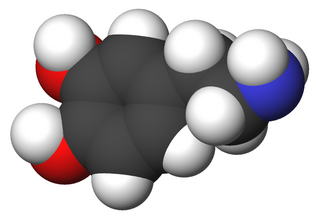
Glucose transporter 1, also known as solute carrier family 2, facilitated glucose transporter member 1 (SLC2A1), is a uniporter protein that in humans is encoded by the SLC2A1 gene. GLUT1 facilitates the transport of glucose across the plasma membranes of mammalian cells. This gene encodes a facilitative glucose transporter that is highly expressed in erythrocytes and endothelial cells, including cells of the blood–brain barrier. The encoded protein is found primarily in the cell membrane and on the cell surface, where it can also function as a receptor for human T-cell leukemia virus (HTLV) I and II. GLUT1 accounts for 2 percent of the protein in the plasma membrane of erythrocytes.
Alternating hemiplegia of childhood (AHC) is an ultra-rare neurological disorder named for the transient episodes, often referred to as "attacks", of hemiplegia that those with the condition experience. It typically presents before the age of 18 months. These hemiplegic attacks can cause anything from mild weakness to complete paralysis on one or both sides of the body, and they can vary greatly in duration. Attacks may also alternate from one side of the body to the other, or alternate between affecting one or both sides during a single attack. Besides hemiplegia, symptoms of the disorder include an extremely broad range of neurological and developmental impairments which are not well understood. Normally, hemiplegia and other associated symptoms cease completely with sleep, but they may recur upon waking.
Episodic ataxia (EA) is an autosomal dominant disorder characterized by sporadic bouts of ataxia with or without myokymia. There are seven types recognized but the majority are due to two recognized entities. Ataxia can be provoked by psychological stress or startle, or heavy exertion, including exercise. Symptoms can first appear in infancy. There are at least six loci for EA, of which 4 are known genes. Some patients with EA also have migraine or progressive cerebellar degenerative disorders, symptomatic of either familial hemiplegic migraine or spinocerebellar ataxia. Some patients respond to acetazolamide though others do not.
Paroxysmal nonkinesigenic dyskinesia (PNKD) is an episodic movement disorder first described by Mount and Reback in 1940 under the name "Familial paroxysmal choreoathetosis". It is a rare hereditary disease that affects various muscular and nervous systems in the body, passing to roughly fifty percent of the offspring.

GLUT1 deficiency syndrome, also known as GLUT1-DS, De Vivo disease or Glucose transporter type 1 deficiency syndrome, is an autosomal dominant genetic metabolic disorder associated with a deficiency of GLUT1, the protein that transports glucose across the blood brain barrier. Glucose Transporter Type 1 Deficiency Syndrome has an estimated birth incidence of 1 in 90,000 to 1 in 24,300. This birth incidence translates to an estimated prevalence of 3,000 to 7,000 in the U.S.
Paroxysmal extreme pain disorder originally named familial rectal pain syndrome, is a rare disorder whose most notable features are pain in the mandibular, ocular and rectal areas as well as flushing. PEPD often first manifests at the beginning of life, perhaps even in utero, with symptoms persisting throughout life. PEPD symptoms are reminiscent of primary erythromelalgia, as both result in flushing and episodic pain, though pain is typically present in the extremities for primary erythromelalgia. Both of these disorders have recently been shown to be allelic, both caused by mutations in the voltage-gated sodium channel NaV1.7 encoded by the gene SCN9A. A different mutation in the SCN9A ion channel causes congenital insensitivity to pain.

PNKD is the abbreviation for a human neurological movement disorder paroxysmal nonkinesiogenic dyskinesia. Like many other human genetics disorders, PNKD also refers to the disease, the disease gene and the encoded protein. (PNKD) is a protein that in humans is encoded by the PNKD gene. Alternative splicing results in the transcription of three isoforms. The mouse ortholog is called brain protein 17 (Brp17).
The paroxysmal dyskinesias (PD) are a group of movement disorders characterized by attacks of hyperkinesia with intact consciousness. Paroxysmal dyskinesia is a rare disorder, however the number of individuals it affects remains unclear. There are three different subtypes of PD that include paroxysmal kinesigenic dyskinesia (PKD), paroxysmal nonkinesigenic dyskinesia (PNKD), and paroxysmal exercise-induced dyskinesia (PED). Other neurological diseases have similar symptoms to PD, such as epilepsy and Parkinson's. The different subtypes make accurate and quick diagnosis of PD challenging. Thus, PD is often under reported and misdiagnosed, making it difficult to accurately study its prevalence in human populations. Onset of PD is usually in late childhood to early adolescence. New drug regimens help treat symptoms of PD, but no cure for the disorder is known.

Paroxysmal exercise-induced dystonia or PED is a rare neurological disorder characterized by sudden, transient, involuntary movements, often including repetitive twisting motions and painful posturing triggered by exercise or other physical exertion. PED is in the class of paroxysmal dyskinesia which are a group of rare movement disorders characterized by attacks of hyperkinesia with intact consciousness. The term paroxysmal indicates that the episodes are sudden and short lived and usually unpredicted, and return to normal is rapid. The number of reported cases of people with PED is very small leading to difficulty in studying and classifying this disease and most studies are limited to a very small number of test subjects.
Dyskinetic cerebral palsy (DCP) is a subtype of cerebral palsy (CP) and is characterized by impaired muscle tone regulation, coordination and movement control. Dystonia and choreoathetosis are the two most dominant movement disorders in patients with DCP.

Infantile convulsions and choreoathetosis (ICCA) syndrome is a neurological genetic disorder with an autosomal dominant mode of inheritance. It is characterized by the association of benign familial infantile epilepsy (BIFE) at age 3–12 months and later in life with paroxysmal kinesigenic choreoathetosis. The ICCA syndrome was first reported in 1997 in four French families from north-western France and provided the first genetic evidence for common mechanisms shared by benign infantile seizures and paroxysmal dyskinesia. The epileptic origin of PKC has long been a matter of debates and PD have been classified as reflex epilepsies. Indeed, attacks of PKC and epileptic seizures have several characteristics in common, they both are paroxysmal in presentation with a tendency to spontaneous remission, and a subset of PKC responds well to anticonvulsants. This genetic disease has been mapped to chromosome 16p-q12. More than 30 families with the clinical characteristics of ICCA syndrome have been described worldwide so far.

Proline-rich transmembrane protein 2 is a protein that in humans is encoded by the PRRT2 gene.
Benign familial infantile epilepsy (BFIE) is an epilepsy syndrome. Affected children, who have no other health or developmental problems, develop seizures during infancy. These seizures have focal origin within the brain but may then spread to become generalised seizures. The seizures may occur several times a day, often grouped in clusters over one to three days followed by a gap of one to three months. Treatment with anticonvulsant drugs is not necessary but they are often prescribed and are effective at controlling the seizures. This form of epilepsy resolves after one or two years, and appears to be completely benign. The EEG of these children, between seizures, is normal. The brain appears normal on MRI scan.
Benign hereditary chorea (BHC), also known as benign familial chorea, is a rare autosomal dominant neurogenetic syndrome. It typically presents itself in childhood with isolated chorea, with average to below average intelligence. Unlike other neurogenetic causes of chorea such as Huntington's disease, BHC is not progressive, and not associated with cognitive decline or psychiatric problems in the vast majority of cases.
Louis Ptáček is an American neurologist and professor who contributed greatly to the field of genetics and neuroscience. He was also an HHMI investigator from 1997 to 2018. His chief areas of research include the understanding of inherited Mendelian disorders and circadian rhythm genes. Currently, Ptáček is a neurology professor and a director of the Division of Neurogenetics in University of California, San Francisco, School of Medicine. His current investigations primarily focus on extensive clinical studies in families with hereditary disorders, which include identifying and characterizing the genes responsible for neurological variations.