Related Research Articles

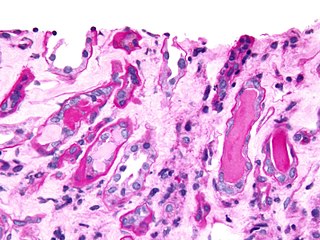
Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.

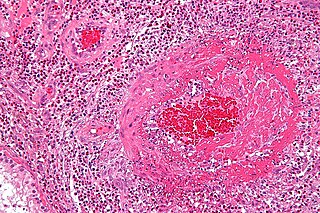
Vasculitis is a group of disorders that destroy blood vessels by inflammation. Both arteries and veins are affected. Lymphangitis is sometimes considered a type of vasculitis. Vasculitis is primarily caused by leukocyte migration and resultant damage. Although both occur in vasculitis, inflammation of veins (phlebitis) or arteries (arteritis) on their own are separate entities.

IgA nephropathy (IgAN), also known as Berger's disease, or synpharyngitic glomerulonephritis, is a disease of the kidney and the immune system; specifically it is a form of glomerulonephritis or an inflammation of the glomeruli of the kidney. Aggressive Berger's disease can attack other major organs, such as the liver, skin and heart.

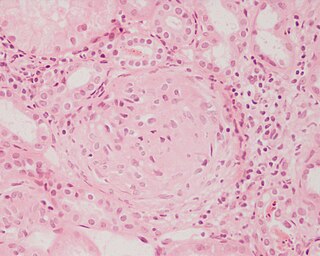
Granulomatosis with polyangiitis (GPA), also known as Wegener's granulomatosis (WG), after the Nazi German physician Friedrich Wegener, is a rare long-term systemic disorder that involves the formation of granulomas and inflammation of blood vessels (vasculitis). It is an autoimmune disease and a form of vasculitis that affects small- and medium-size vessels in many organs but most commonly affects the upper respiratory tract, lungs and kidneys. The signs and symptoms of GPA are highly varied and reflect which organs are supplied by the affected blood vessels. Typical signs and symptoms include nosebleeds, stuffy nose and crustiness of nasal secretions, and inflammation of the uveal layer of the eye. Damage to the heart, lungs and kidneys can be fatal.
Eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as allergic granulomatosis, is an extremely rare autoimmune condition that causes inflammation of small and medium-sized blood vessels (vasculitis) in persons with a history of airway allergic hypersensitivity (atopy).
Glomerulonephritis (GN) is a term used to refer to several kidney diseases. Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the name, but not all diseases necessarily have an inflammatory component.

Anti-neutrophil cytoplasmic antibodies (ANCAs) are a group of autoantibodies, mainly of the IgG type, against antigens in the cytoplasm of neutrophils and monocytes. They are detected as a blood test in a number of autoimmune disorders, but are particularly associated with systemic vasculitis, so called ANCA-associated vasculitides (AAV).

Nephritic syndrome is a syndrome comprising signs of nephritis, which is kidney disease involving inflammation. It often occurs in the glomerulus, where it is called glomerulonephritis. Glomerulonephritis is characterized by inflammation and thinning of the glomerular basement membrane and the occurrence of small pores in the podocytes of the glomerulus. These pores become large enough to permit both proteins and red blood cells to pass into the urine. By contrast, nephrotic syndrome is characterized by proteinuria and a constellation of other symptoms that specifically do not include hematuria. Nephritic syndrome, like nephrotic syndrome, may involve low level of albumin in the blood due to the protein albumin moving from the blood to the urine.
Microscopic polyangiitis is an autoimmune disease characterized by a systemic, pauci-immune, necrotizing, small-vessel vasculitis without clinical or pathological evidence of granulomatous inflammation.
Eosinophiluria is the abnormal presence of eosinophils in the urine. It can be measured by detecting levels of eosinophil cationic protein.
Urinary casts are microscopic cylindrical structures produced by the kidney and present in the urine in certain disease states. They form in the distal convoluted tubule and collecting ducts of nephrons, then dislodge and pass into the urine, where they can be detected by microscopy.

p-ANCA, or MPO-ANCA, or perinuclear anti-neutrophil cytoplasmic antibodies, are antibodies that stain the material around the nucleus of a neutrophil. They are a special class of anti-neutrophil cytoplasmic antibodies.

Rapidly progressive glomerulonephritis (RPGN) is a syndrome of the kidney that is characterized by a rapid loss of kidney function, with glomerular crescent formation seen in at least 50% or 75% of glomeruli seen on kidney biopsies. If left untreated, it rapidly progresses into acute kidney failure and death within months. In 50% of cases, RPGN is associated with an underlying disease such as Goodpasture syndrome, systemic lupus erythematosus or granulomatosis with polyangiitis; the remaining cases are idiopathic. Regardless of the underlying cause, RPGN involves severe injury to the kidneys' glomeruli, with many of the glomeruli containing characteristic glomerular crescents.
An overlap syndrome is a medical condition which shares features of at least two more widely recognised disorders. Examples of overlap syndromes can be found in many medical specialties such as overlapping connective tissue disorders in rheumatology, and overlapping genetic disorders in cardiology.

Mesangial proliferative glomerulonephritis (MesPGN) is a morphological pattern characterized by a numerical increase in mesangial cells and expansion of the extracellular matrix within the mesangium of the glomerulus. The increase in the number of mesangial cells can be diffuse or local and immunoglobulin and/or complement deposition can also occur. MesPGN is associated with a variety of disease processes affecting the glomerulus, though can be idiopathic. The clinical presentation of MesPGN usually consists of hematuria or nephrotic syndrome. Treatment is often consistent with the histologic pattern of and/or disease process contributing to mesangial proliferative glomerulonephritis, and usually involves some form of immunosuppressant.
Pulmonary-renal syndrome (PRS) is a rare medical syndrome in which respiratory failure involving bleeding in the lungs and kidney failure (glomerulonephritis) occur. PRS is associated with a high rate of morbidity and death. The term was first used by Goodpasture in 1919 to describe the association of respiratory and kidney failure.
Necrotizing vasculitis, also called systemic necrotizing vasculitus, is a category of vasculitis, comprising vasculitides that present with necrosis. Examples include giant cell arteritis, microscopic polyangiitis, and granulomatosis with polyangiitis. ICD-10 uses the variant "necrotizing vasculopathy". ICD-9, while classifying these conditions together, does not use a dedicated phrase, instead calling them "polyarteritis nodosa and allied conditions".
Diffuse proliferative glomerulonephritis (DPGN) is a type of glomerulonephritis that is the most serious form of renal lesions in SLE and is also the most common, occurring in 35% to 60% of patients. In absence of SLE, DPGN pathology looks more like Membranoproliferative glomerulonephritis
Vasculitic neuropathy is a peripheral neuropathic disease. In a vasculitic neuropathy there is damage to the vessels that supply blood to the nerves. It can be as part of a systemic problem or can exist as a single-organ issue only affecting the peripheral nervous system (PNS). It is diagnosed with the use of electrophysiological testing, blood tests, nerve biopsy and clinical examination. It is a serious medical condition that can cause prolonged morbidity and disability and generally requires treatment. Treatment depends on the type but it is mostly with corticosteroids or immunomodulating therapies.
Monoclonal gammopathy of renal significance (MGRS) are a group of kidney disorders that present with kidney damage due to nephrotoxic monoclonal immunoglobulins secreted by clonal plasma cells or B cells. By definition, people with MGRS do not meet criteria for multiple myeloma or other hematologic malignancies. The term MGRS was introduced in 2012 by the International Kidney and Monoclonal Gammopathy Research Group (IKMG). MGRS is associated with monoclonal gammopathy of undetermined significance (MGUS). People with MGUS have a monoclonal gammopathy but does not meet the criteria for the clonal burden nor the presence of end organ damage seen in hematologic malignancies. In a population based study based on the NHANES III health survey; 6% of patients with MGUS were subsequently classified as having MGRS. The prevalence and incidence of MGRS in the general population or in specific populations is not known but it is more prevalent in those over the age of 50 as there is a monoclonal protein (M-protein) present in 3% of those 50 and years older and 5% of those 70 years and older, placing those 50 and older at increased risk of MGRS.
References
- 1 2 3 4 5 Sattar (2011). Fundamentals of Pathology. p. 130. ISBN 978-0983224600.
- ↑ "Final Diagnosis -- Case 51" . Retrieved 2009-06-08.
- ↑ Bollée G, Noël LH, Suarez F, et al. (June 2009). "Pauci-immune crescentic glomerulonephritis associated with ANCA of IgA class". Am. J. Kidney Dis. 53 (6): 1063–7. doi:10.1053/j.ajkd.2008.10.039. PMID 19084310.