Crohn's disease is a type of inflammatory bowel disease (IBD) that may affect any segment of the gastrointestinal tract. Symptoms often include abdominal pain, diarrhea, fever, abdominal distension, and weight loss. Complications outside of the gastrointestinal tract may include anemia, skin rashes, arthritis, inflammation of the eye, and fatigue. The skin rashes may be due to infections as well as pyoderma gangrenosum or erythema nodosum. Bowel obstruction may occur as a complication of chronic inflammation, and those with the disease are at greater risk of colon cancer and small bowel cancer.

Ulcerative colitis (UC) is one of the two types of inflammatory bowel disease (IBD), with the other main type being Crohn’s disease. It is a long-term condition that results in inflammation and ulcers of the colon and rectum. The primary symptoms of active disease are abdominal pain and diarrhea mixed with blood (hematochezia). Weight loss, fever, and anemia may also occur. Often, symptoms come on slowly and can range from mild to severe. Symptoms typically occur intermittently with periods of no symptoms between flares. Complications may include abnormal dilation of the colon (megacolon), inflammation of the eye, joints, or liver, and colon cancer.

Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, with Crohn's disease and ulcerative colitis (UC) being the principal types. Crohn's disease affects the small intestine and large intestine, as well as the mouth, esophagus, stomach and the anus, whereas ulcerative colitis primarily affects the colon and the rectum.

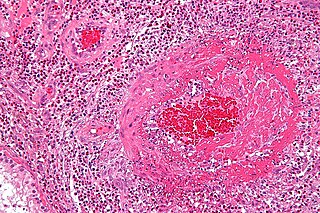
Vasculitis is a group of disorders that destroy blood vessels by inflammation. Both arteries and veins are affected. Lymphangitis is sometimes considered a type of vasculitis. Vasculitis is primarily caused by leukocyte migration and resultant damage. Although both occur in vasculitis, inflammation of veins (phlebitis) or arteries (arteritis) on their own are separate entities.

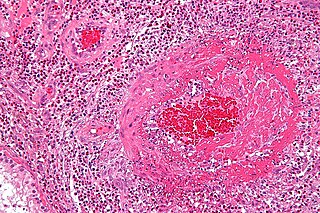
Granulomatosis with polyangiitis (GPA), also known as Wegener's granulomatosis (WG), after the German physician Friedrich Wegener, is a rare long-term systemic disorder that involves the formation of granulomas and inflammation of blood vessels (vasculitis). It is an autoimmune disease and a form of vasculitis that affects small- and medium-size vessels in many organs but most commonly affects the upper respiratory tract, lungs and kidneys. The signs and symptoms of GPA are highly varied and reflect which organs are supplied by the affected blood vessels. Typical signs and symptoms include nosebleeds, stuffy nose and crustiness of nasal secretions, and inflammation of the uveal layer of the eye. Damage to the heart, lungs and kidneys can be fatal.
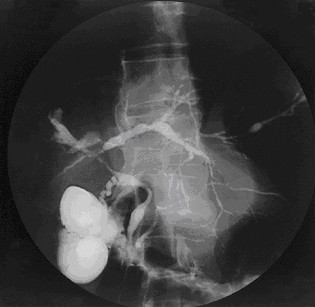
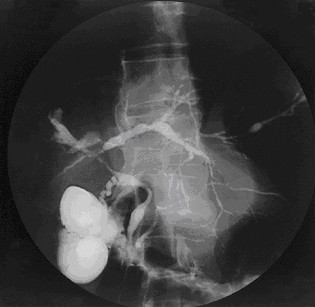
Primary sclerosing cholangitis (PSC) is a long-term progressive disease of the liver and gallbladder characterized by inflammation and scarring of the bile ducts, which normally allow bile to drain from the gallbladder. Affected individuals may have no symptoms or may experience signs and symptoms of liver disease, such as yellow discoloration of the skin and eyes, itching, and abdominal pain.
Eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as allergic granulomatosis, is an extremely rare autoimmune condition that causes inflammation of small and medium-sized blood vessels (vasculitis) in persons with a history of airway allergic hypersensitivity (atopy).
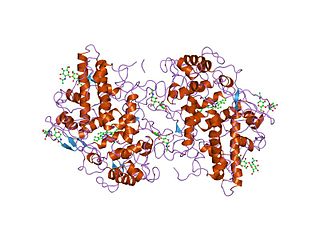
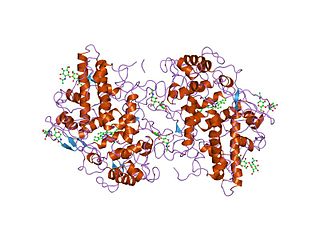
Myeloperoxidase (MPO) is a peroxidase enzyme that in humans is encoded by the MPO gene on chromosome 17. MPO is most abundantly expressed in neutrophils, and produces hypohalous acids to carry out their antimicrobial activity, including hypochlorous acid, the sodium salt of which is the chemical in bleach. It is a lysosomal protein stored in azurophilic granules of the neutrophil and released into the extracellular space during degranulation. Neutrophil myeloperoxidase has a heme pigment, which causes its green color in secretions rich in neutrophils, such as mucus and sputum. The green color contributed to its outdated name verdoperoxidase.

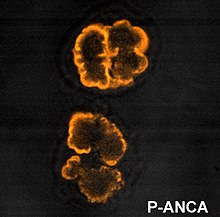
Anti-neutrophil cytoplasmic antibodies (ANCAs) are a group of autoantibodies, mainly of the IgG type, against antigens in the cytoplasm of neutrophils and monocytes. They are detected as a blood test in a number of autoimmune disorders, but are particularly associated with systemic vasculitis, so called ANCA-associated vasculitides (AAV).
Microscopic polyangiitis is an autoimmune disease characterized by a systemic, pauci-immune, necrotizing, small-vessel vasculitis without clinical or pathological evidence of granulomatous inflammation.

c-ANCAs, or PR3-ANCA, or antineutrophil cytoplasmic antibodies, are a type of autoantibody, an antibody produced by the body that acts against one of its own proteins. These antibodies show a diffusely granular, cytoplasmic staining pattern under microscopy. This pattern results from binding of ANCAs to antigen targets throughout the neutrophil cytoplasm, the most common protein target being proteinase 3 (PR3). For example, PR3 is the most common antigen target of ANCA in patients with granulomatosis with polyangiitis. In active granulomatosis with polyangiitis, c-ANCA is found over 90% of the time. Other antigens may also occasionally result in a c-ANCA pattern.

Biological therapy, the use of medications called biopharmaceuticals or biologics that are tailored to specifically target an immune or genetic mediator of disease, plays a major role in the treatment of inflammatory bowel disease. Even for diseases of unknown cause, molecules that are involved in the disease process have been identified, and can be targeted for biological therapy. Many of these molecules, which are mainly cytokines, are directly involved in the immune system. Biological therapy has found a niche in the management of cancer, autoimmune diseases, and diseases of unknown cause that result in symptoms due to immune related mechanisms.

Rapidly progressive glomerulonephritis (RPGN) is a syndrome of the kidney that is characterized by a rapid loss of kidney function, with glomerular crescent formation seen in at least 50% or 75% of glomeruli seen on kidney biopsies. If left untreated, it rapidly progresses into acute kidney failure and death within months. In 50% of cases, RPGN is associated with an underlying disease such as Goodpasture syndrome, systemic lupus erythematosus or granulomatosis with polyangiitis; the remaining cases are idiopathic. Regardless of the underlying cause, RPGN involves severe injury to the kidneys' glomeruli, with many of the glomeruli containing characteristic glomerular crescents.
Anti-Saccharomyces cerevisiae antibodies (ASCAs) are antibodies against antigens presented by the cell wall of the yeast Saccharomyces cerevisiae. These antibodies are directed against oligomannose sequences α-1,3 Man n. ASCAs and perinuclear antineutrophil cytoplasmic antibodies (pANCAs) are the two most useful and often discriminating biomarkers for colitis. ASCA tends to recognize Crohn's disease more frequently, whereas pANCA tend to recognize ulcerative colitis.
Vedolizumab, sold under the brand name Entyvio, is a monoclonal antibody medication developed by Millennium Pharmaceuticals, Inc. for the treatment of ulcerative colitis and Crohn's disease. It binds to integrin α4β7, blocking the α4β7 integrin results in gut-selective anti-inflammatory activity.
Faecal calprotectin is a biochemical measurement of the protein calprotectin in the stool. Elevated faecal calprotectin indicates the migration of neutrophils to the intestinal mucosa, which occurs during intestinal inflammation, including inflammation caused by inflammatory bowel disease. Under a specific clinical scenario, the test may eliminate the need for invasive colonoscopy or radio-labelled white cell scanning.

Necrotizing vasculitis, also called systemic necrotizing vasculitis, is a general term for the inflammation of veins and arteries that develops into necrosis and narrows the vessels.

Enteropathic arthropathy commonly referred to as enteropathic arthritis, is a type of arthritis linked to Crohn's disease, ulcerative colitis, and chronic inflammatory bowel diseases.
Ronald Jonathan Falk, MD, FACP, FASN is the Nan and Hugh Cullman Eminent Professor and Chair of the Department of Medicine at the University of North Carolina-Chapel Hill (UNC). He is a clinical nephrologist and internationally recognized expert in anti-neutrophil cytoplasmic autoantibody (ANCA)-induced vasculitis and autoimmune kidney disease. His career as a translational physician-scientist spans more than three decades. His clinical practice and translational research focus on characterizing the cell, tissue and physiologic changes in the development of specific autoimmune kidney diseases and developing new approaches for studying autoimmunity, inflammation and basic neutrophil/monocyte biology. He was Chief of the UNC Division of Nephrology and Hypertension from 1993-2015. He co-founded the UNC Kidney Center in 2005 and continues as Co-Director. Falk is a Past-President of the American Society of Nephrology (ASN). Since 2015, he has served as Chair of the Department of Medicine at UNC.
Shomron Ben-Horin is an Israeli physician, a co-founder & Chief Medical Officer of Evinature, and professor of medicine at the Tel-Aviv University.