It is proposed that this article be deleted because of the following concern:
If you can address this concern by improving, copyediting, sourcing, renaming, or merging the page, please edit this page and do so. You may remove this message if you improve the article or otherwise object to deletion for any reason. Although not required, you are encouraged to explain why you object to the deletion, either in your edit summary or on the talk page. If this template is removed, do not replace it . The article may be deleted if this message remains in place for seven days, i.e., after 00:25, 27 February 2025 (UTC). Find sources: "Anti-centromere antibodies" – news · newspapers · books · scholar · JSTOR Nominator: Please consider notifying the author/project: {{ subst:proposed deletion notify |Anti-centromere antibodies|concern=this article doesn't really contain any information that's not already available at [[Antinuclear antibody]] and unfortunately resources about this specific antibody are not easy to find}} ~~~~ |

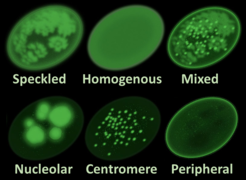
Anti-centromere antibodies (ACAs; often styled solid, anticentromere) are autoantibodies specific to centromere and kinetochore function. They occur in some autoimmune diseases, frequently in limited systemic scleroderma (formerly called CREST syndrome), and occasionally in the diffuse form of scleroderma. They are rare in other rheumatic diseases and in healthy persons.
Anti-centromere antibodies are found in approximately 60% of patients with limited systemic scleroderma and in 15% of those with the diffuse form of scleroderma. The specificity of this test is >98%. Thus, a positive anti-centromere antibody finding is strongly suggestive of limited systemic scleroderma. Anti-centromere antibodies present early in the course of disease and are notably predictive of limited cutaneous involvement and a decreased likelihood of aggressive internal organ involvement, such as fibrosis in the lungs. [1]
When present in primary biliary cirrhosis, ACAs are prognostic of portal hypertension such that serum ACA levels correlate with the severity of portal hypertension. [2]
- A schematic representation of an antibody