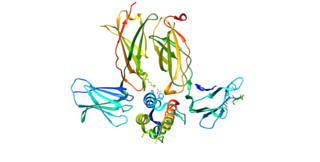
A dendritic cell (DC) is an antigen-presenting cell of the mammalian immune system. A DC's main function is to process antigen material and present it on the cell surface to the T cells of the immune system. They act as messengers between the innate and adaptive immune systems.

The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

Dry eye syndrome, also known as keratoconjunctivitis sicca, is the condition of having dry eyes. Symptoms include dryness in the eye, irritation, redness, discharge, blurred vision, and easily fatigued eyes. Symptoms range from mild and occasional to severe and continuous. Dry eye syndrome can lead to blurred vision, instability of the tear film, increased risk of damage to the ocular surface such as scarring of the cornea, and changes in the eye including the neurosensory system.
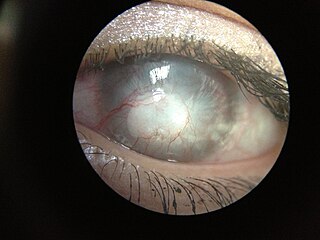
Uveitis is inflammation of the uvea, the pigmented layer of the eye between the inner retina and the outer fibrous layer composed of the sclera and cornea. The uvea consists of the middle layer of pigmented vascular structures of the eye and includes the iris, ciliary body, and choroid. Uveitis is described anatomically, by the part of the eye affected, as anterior, intermediate or posterior, or panuveitic if all parts are involved. Anterior uveitis (iridocyclitis) is the most common, with the incidence of uveitis overall affecting approximately 1:4500, most commonly those between the ages of 20-60. Symptoms include eye pain, eye redness, floaters and blurred vision, and ophthalmic examination may show dilated ciliary blood vessels and the presence of cells in the anterior chamber. Uveitis may arise spontaneously, have a genetic component, or be associated with an autoimmune disease or infection. While the eye is a relatively protected environment, its immune mechanisms may be overcome resulting in inflammation and tissue destruction associated with T-cell activation.

A Langerhans cell (LC) is a tissue-resident macrophage of the skin once thought to be a resident dendritic cell. These cells contain organelles called Birbeck granules. They are present in all layers of the epidermis and are most prominent in the stratum spinosum. They also occur in the papillary dermis, particularly around blood vessels, as well as in the mucosa of the mouth, foreskin, and vaginal epithelium. They can be found in other tissues, such as lymph nodes, particularly in association with the condition Langerhans cell histiocytosis (LCH).

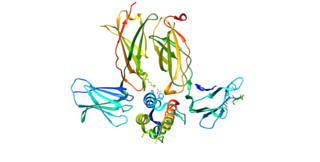
Lacritin is a 12.3 kDa glycoprotein encoded in humans by the LACRT gene. Lacritin's discovery emerged from a screen for factors that stimulate tear protein secretion. Lacritin is a secreted protein found in tears and saliva. Lacritin also promotes tear secretion, the proliferation and survival of epithelial cells, and corneal wound healing Lacritin is thus a multifunctional prosecretory mitogen with cell survival activity. Natural or bacterial cleavage of lacritin releases a C-terminal fragment that is bactericidal.
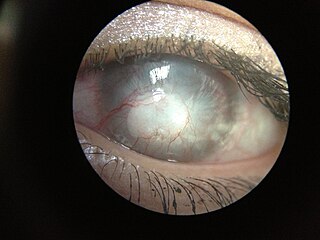
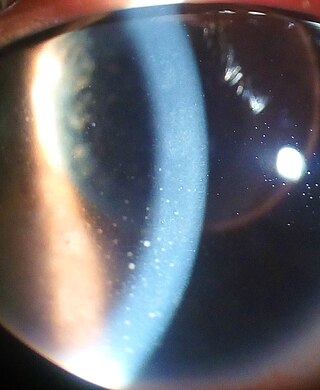
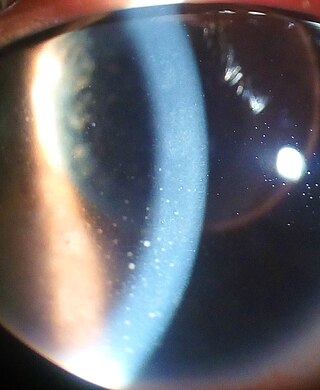
Corneal neovascularization (CNV) is the in-growth of new blood vessels from the pericorneal plexus into avascular corneal tissue as a result of oxygen deprivation. Maintaining avascularity of the corneal stroma is an important aspect of corneal pathophysiology as it is required for corneal transparency and optimal vision. A decrease in corneal transparency causes visual acuity deterioration. Corneal tissue is avascular in nature and the presence of vascularization, which can be deep or superficial, is always pathologically related.

Langerin (CD207) is a type II transmembrane protein which is encoded by the CD207 gene in humans. It was discovered by scientists Sem Saeland and Jenny Valladeau as a main part of Birbeck granules. Langerin is C-type lectin receptor on Langerhans cells (LCs) and in mice also on dermal interstitial CD103+ dendritic cells (DC) and on resident CD8+ DC in lymph nodes.

Chronic superficial keratitis (CSK), also known as pannus or Uberreiter's disease, is an inflammatory condition of the cornea in dogs, particularly seen in the German Shepherd. Both eyes are usually affected. The corneas gradually become pigmented and infiltrated by blood vessels, and the dog may eventually become blind.
Certain sites of the mammalian body have immune privilege, meaning they are able to tolerate the introduction of antigens without eliciting an inflammatory immune response. Tissue grafts are normally recognised as foreign antigens by the body and attacked by the immune system. However, in immune privileged sites, tissue grafts can survive for extended periods of time without rejection occurring. Immunologically privileged sites include:
Thymic stromal lymphopoietin (TSLP) is a protein belonging to the cytokine family. It is known to play an important role in the maturation of T cell populations through activation of antigen-presenting cells.

The ocular immune system protects the eye from infection and regulates healing processes following injuries. The interior of the eye lacks lymph vessels but is highly vascularized, and many immune cells reside in the uvea, including mostly macrophages, dendritic cells, and mast cells. These cells fight off intraocular infections, and intraocular inflammation can manifest as uveitis or retinitis. The cornea of the eye is immunologically a very special tissue. Its constant exposure to the exterior world means that it is vulnerable to a wide range of microorganisms while its moist mucosal surface makes the cornea particularly susceptible to attack. At the same time, its lack of vasculature and relative immune separation from the rest of the body makes immune defense difficult. Lastly, the cornea is a multifunctional tissue. It provides a large part of the eye's refractive power, meaning it has to maintain remarkable transparency, but must also serve as a barrier to keep pathogens from reaching the rest of the eye, similar to function of the dermis and epidermis in keeping underlying tissues protected. Immune reactions within the cornea come from surrounding vascularized tissues as well as innate immune responsive cells that reside within the cornea.

Gholam A. Peyman is an Iranian American ophthalmologist, retina surgeon, and inventor. He is best known for his invention of LASIK eye surgery, a vision correction procedure designed to allow people to see clearly without glasses. He was awarded the first US patent for the procedure in 1989.

Herpetic simplex keratitis is a form of keratitis caused by recurrent herpes simplex virus (HSV) infection in the cornea.

Reza Dana is the Claes H. Dohlman Professor of Ophthalmology, senior scientist and W. Clement Stone Clinical Research Scholar at Massachusetts Eye and Ear, Harvard Medical School, and director of the Harvard-Vision Clinical Scientist Development Program.
Gerd Geerling is a German consultant ophthalmic surgeon, Professor of Ophthalmology and since 2011 head of the Universitäts-Augenklinik Düsseldorf of the University of Düsseldorf, Germany.
Aganirsen is a 25 mer DNA antisense oligonucleotide therapeutic inhibiting insulin receptor substrate-1 (IRS-1), which is being investigated as a topical treatment for ocular neovascularization. Aganirsen is a candidate for the treatment of ocular neovascularization in patients with front of the eye (cornea) or back of the eye (retinal) diseases, including progressive corneal neovascularization in patients with infectious keratitis and wet age related macular degeneration (AMD).
Mooren's ulcer is a rare idiopathic ocular disorder that may lead to blindness due to progressive destruction of the peripheral cornea. Although the etiology of Mooren's ulcer is poorly understood, recent evidence suggests that the pathogenesis of this disease appears to be the result of an autoimmune process directed against molecules expressed in the corneal stroma.

Alireza Mashaghi is a physician-scientist and biophysicist at Leiden University. He is known for his contributions to single-molecule analysis of chaperone assisted protein folding, molecular topology and medical systems biophysics and bioengineering. He is a leading advocate for interdisciplinary research and education in medicine and pharmaceutical sciences.

The human cornea is a transparent membrane which allows light to pass through it. The word corneal opacification literally means loss of normal transparency of cornea. The term corneal opacity is used particularly for the loss of transparency of cornea due to scarring. Transparency of the cornea is dependent on the uniform diameter and the regular spacing and arrangement of the collagen fibrils within the stroma. Alterations in the spacing of collagen fibrils in a variety of conditions including corneal edema, scars, and macular corneal dystrophy is clinically manifested as corneal opacity. The term corneal blindness is commonly used to describe blindness due to corneal opacity.