The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth. Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.

Pre-eclampsia is a multi-system disorder specific to pregnancy, characterized by the onset of high blood pressure and often a significant amount of protein in the urine. When it arises, the condition begins after 20 weeks of pregnancy. In severe cases of the disease there may be red blood cell breakdown, a low blood platelet count, impaired liver function, kidney dysfunction, swelling, shortness of breath due to fluid in the lungs, or visual disturbances. Pre-eclampsia increases the risk of undesirable as well as lethal outcomes for both the mother and the fetus including preterm labor. If left untreated, it may result in seizures at which point it is known as eclampsia.

Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening. Symptoms include vaginal bleeding in the second half of pregnancy. The bleeding is bright red and tends not to be associated with pain. Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery. Complications for the baby may include fetal growth restriction.

Placentophagy, also known as placentophagia, is the act of consuming part or all of the afterbirth following parturition in mammals. Parturition involves the delivery of the neonate, as well as the placenta and fetal membranes. The placenta is a critical organ that develops in the maternal uterus during pregnancy to support the fetus. It connects to the fetus via the umbilical cord in order to allow nutrient transport, waste excretion and gas exchange between mother and fetus. The morphological features of the placenta differ among species, but the function is universal. The behaviour is characteristic to the mother of the majority of placental mammals. Significant documentation has been provided on placentophagy in a range of animals.

Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
Antepartum bleeding, also known as antepartum haemorrhage (APH) or prepartum hemorrhage, is genital bleeding during pregnancy after the 28th week of pregnancy up to delivery.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

Intrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. It may be due to a variety of reasons such as prolapse or occlusion of the umbilical cord, placental infarction, maternal diabetes and maternal smoking. Intrauterine growth restriction may cause or be the result of hypoxia. Intrauterine hypoxia can cause cellular damage that occurs within the central nervous system. This results in an increased mortality rate, including an increased risk of sudden infant death syndrome (SIDS). Oxygen deprivation in the fetus and neonate have been implicated as either a primary or as a contributing risk factor in numerous neurological and neuropsychiatric disorders such as epilepsy, attention deficit hyperactivity disorder, eating disorders and cerebral palsy.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.

Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood following childbirth. Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist. Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and an increased breathing rate. As more blood is lost, the patient may feel cold, blood pressure may drop, and they may become restless or unconscious. The condition can occur up to six weeks following delivery.
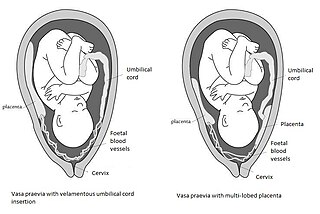
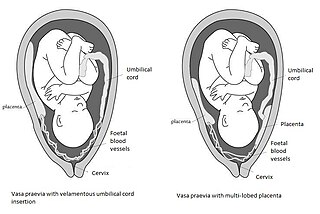
Vasa praevia is a condition in which fetal blood vessels cross or run near the internal opening of the uterus. These vessels are at risk of rupture when the supporting membranes rupture, as they are unsupported by the umbilical cord or placental tissue.

Peroxisome proliferator-activated receptor gamma, also known as the glitazone reverse insulin resistance receptor, or NR1C3 is a type II nuclear receptor functioning as a transcription factor that in humans is encoded by the PPARG gene.

Placental growth factor(PlGF) is a protein that in humans is encoded by the PGF gene.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.

Ubenimex (INN), also known more commonly as bestatin, is a competitive, reversible protease inhibitor. It is an inhibitor of arginyl aminopeptidase (aminopeptidase B), leukotriene A4 hydrolase (a zinc metalloprotease that displays both epoxide hydrolase and aminopeptidase activities), alanyl aminopeptidase (aminopeptidase M/N), leucyl/cystinyl aminopeptidase (oxytocinase/vasopressinase), and membrane dipeptidase (leukotriene D4 hydrolase). It is being studied for use in the treatment of acute myelocytic leukemia and lymphedema. It is derived from Streptomyces olivoreticuli. Ubenimex has been found to inhibit the enzymatic degradation of oxytocin, vasopressin, enkephalins, and various other peptides and compounds.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.
Tobacco smoking during pregnancy causes many detrimental effects on health and reproduction, in addition to the general health effects of tobacco. A number of studies have shown that tobacco use is a significant factor in miscarriages among pregnant smokers, and that it contributes to a number of other threats to the health of the foetus.

Human placentophagy, or consumption of the placenta, is defined as "the ingestion of a human placenta postpartum, at any time, by any person, either in raw or altered form". While there are several anecdotes of different cultures practicing placentophagy in varying contexts, maternal placentophagy started in the US in the 1970s, with little to no evidence of its practice in any traditional or historic culture. Midwives and alternative-health advocates in the U.S. are the primary groups encouraging post-partum maternal placentophagy.

The placental microbiome is the nonpathogenic, commensal bacteria claimed to be present in a healthy human placenta and is distinct from bacteria that cause infection and preterm birth in chorioamnionitis. Until recently, the healthy placenta was considered to be a sterile organ but now genera and species have been identified that reside in the basal layer.