A pulmonary alveolus, also known as an air sac or air space, is one of millions of hollow, distensible cup-shaped cavities in the lungs where oxygen is exchanged for carbon dioxide. Alveoli make up the functional tissue of the mammalian lungs known as the lung parenchyma, which takes up 90 percent of the total lung volume.
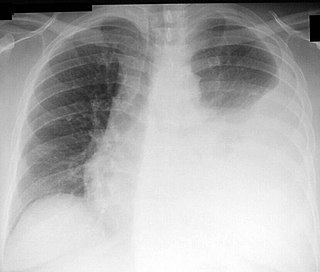
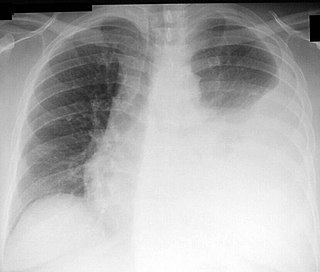
Radiology (X-rays) is used in the diagnosis of tuberculosis. Abnormalities on chest radiographs may be suggestive of, but are never diagnostic of TB, but can be used to rule out pulmonary TB.

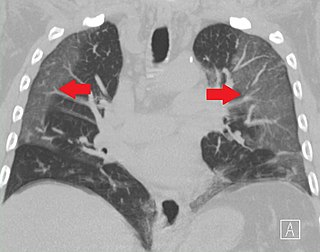
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in medicine.

A pulmonary sequestration is a medical condition wherein a piece of tissue that ultimately develops into lung tissue is not attached to the pulmonary arterial blood supply, as is the case in normally developing lung. This sequestered tissue is therefore not connected to the normal bronchial airway architecture, and fails to function in, and contribute to, respiration of the organism.
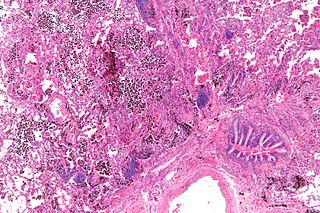
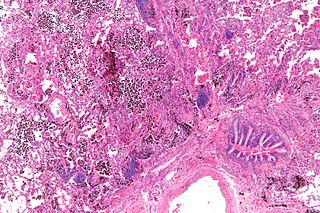
Pulmonary hemorrhage is an acute bleeding from the lung, from the upper respiratory tract and the trachea, and the pulmonary alveoli. When evident clinically, the condition is usually massive. The onset of pulmonary hemorrhage is characterized by a cough productive of blood (hemoptysis) and worsening of oxygenation leading to cyanosis. Treatment should be immediate and should include tracheal suction, oxygen, positive pressure ventilation, and correction of underlying abnormalities such as disorders of coagulation. A blood transfusion may be necessary.

Hypersensitivity pneumonitis (HP) or extrinsic allergic alveolitis (EAA) is a syndrome caused by the repetitive inhalation of antigens from the environment in susceptible or sensitized people. Common antigens include molds, bacteria, bird droppings, bird feathers, agricultural dusts, bioaerosols and chemicals from paints or plastics. People affected by this type of lung inflammation (pneumonitis) are commonly exposed to the antigens by their occupations, hobbies, the environment and animals. The inhaled antigens produce a hypersensitivity immune reaction causing inflammation of the airspaces (alveoli) and small airways (bronchioles) within the lung. Hypersensitivity pneumonitis may eventually lead to interstitial lung disease.
Thoracentesis, also known as thoracocentesis, pleural tap, needle thoracostomy, or needle decompression, is an invasive medical procedure to remove fluid or air from the pleural space for diagnostic or therapeutic purposes. A cannula, or hollow needle, is carefully introduced into the thorax, generally after administration of local anesthesia. The procedure was first performed by Morrill Wyman in 1850 and then described by Henry Ingersoll Bowditch in 1852.

Lipoid pneumonia is a specific form of lung inflammation (pneumonia) that develops when lipids enter the bronchial tree. The disorder is sometimes called cholesterol pneumonia in cases where that lipid is a factor.
Restrictive lung diseases are a category of extrapulmonary, pleural, or parenchymal respiratory diseases that restrict lung expansion, resulting in a decreased lung volume, an increased work of breathing, and inadequate ventilation and/or oxygenation. Pulmonary function test demonstrates a decrease in the forced vital capacity.

A pulmonary contusion, also known as lung contusion, is a bruise of the lung, caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in the lung tissue. The excess fluid interferes with gas exchange, potentially leading to inadequate oxygen levels (hypoxia). Unlike pulmonary laceration, another type of lung injury, pulmonary contusion does not involve a cut or tear of the lung tissue.

A pulmonary laceration is a chest injury in which lung tissue is torn or cut. An injury that is potentially more serious than pulmonary contusion, pulmonary laceration involves disruption of the architecture of the lung, while pulmonary contusion does not. Pulmonary laceration is commonly caused by penetrating trauma but may also result from forces involved in blunt trauma such as shear stress. A cavity filled with blood, air, or both can form. The injury is diagnosed when collections of air or fluid are found on a CT scan of the chest. Surgery may be required to stitch the laceration, to drain blood, or even to remove injured parts of the lung. The injury commonly heals quickly with few problems if it is given proper treatment; however it may be associated with scarring of the lung or other complications.

Tracheobronchial injury is damage to the tracheobronchial tree. It can result from blunt or penetrating trauma to the neck or chest, inhalation of harmful fumes or smoke, or aspiration of liquids or objects.

A lung nodule or pulmonary nodule is a relatively small focal density in the lung. A solitary pulmonary nodule (SPN) or coin lesion, is a mass in the lung smaller than three centimeters in diameter. A pulmonary micronodule has a diameter of less than three millimetres. There may also be multiple nodules.
A pulmonary hematoma is a collection of blood within the tissue of the lung. It may result when a pulmonary laceration fills with blood. A lung laceration filled with air is called a pneumatocele. In some cases, both pneumatoceles and hematomas exist in the same injured lung. Pulmonary hematomas take longer to heal than simple pneumatoceles and commonly leave the lungs scarred. A pulmonary contusion is another cause of bleeding within the lung tissue, but these result from microhemorrhages, multiple small bleeds, and the bleeding is not a discrete mass but rather occurs within the lung tissue. An indication of more severe damage to the lung than pulmonary contusion, a hematoma also takes longer to clear. Unlike contusions, hematomas do not usually interfere with gas exchange in the lung, but they do increase the risk of infection and abscess formation.
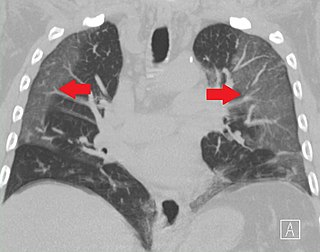
Ground-glass opacity (GGO) is a finding seen on chest x-ray (radiograph) or computed tomography (CT) imaging of the lungs. It is typically defined as an area of hazy opacification (x-ray) or increased attenuation (CT) due to air displacement by fluid, airway collapse, fibrosis, or a neoplastic process. When a substance other than air fills an area of the lung it increases that area's density. On both x-ray and CT, this appears more grey or hazy as opposed to the normally dark-appearing lungs. Although it can sometimes be seen in normal lungs, common pathologic causes include infections, interstitial lung disease, and pulmonary edema.

Fire breather's pneumonia is a distinct type of exogenous—that is, originating outside the body—lipoid pneumonia that results from inhalation or aspiration of hydrocarbons of different types, such as lamp oil. Accidental inhalation of hydrocarbon fuels can occur during fire breathing, fire eating, or other fire performance, and may lead to pneumonitis.
Hydrocarbon pneumonitis is a kind of chemical pneumonitis which occurs with oral ingestion of hydrocarbons and associated aspiration. It occurs prominently among children, accounting for many hospital admissions each year. Common hydrocarbons involved are mineral spirits, mineral seal oil, lamp oil, kerosene (paraffin), turpentine, gasoline, and lighter fluid. Pneumatocele is a complication of hydrocarbon pneumonitis. In both childhood and adult pneumonitis, hydrocarbon aspiration occurs at the time of initial ingestion event or subsequently with vomiting. Low viscosity of an ingested hydrocarbon is considered a major factor promoting aspiration. Contrary to aspiration hydrocarbon pneumonitis, hydrocarbon (solvent) vapor inhalation manifests primarily in either central nervous system or cardiac effects.

A lung cavity or pulmonary cavity is an abnormal, thick-walled, air-filled space within the lung. Cavities in the lung can be caused by infections, cancer, autoimmune conditions, trauma, congenital defects, or pulmonary embolism. The most common cause of a single lung cavity is lung cancer. Bacterial, mycobacterial, and fungal infections are common causes of lung cavities. Globally, tuberculosis is likely the most common infectious cause of lung cavities. Less commonly, parasitic infections can cause cavities. Viral infections almost never cause cavities. The terms cavity and cyst are frequently used interchangeably; however, a cavity is thick walled, while a cyst is thin walled. The distinction is important because cystic lesions are unlikely to be cancer, while cavitary lesions are often caused by cancer.

A focal lung pneumatosis, is an enclosed pocket of air or gas in the lung and includes blebs, bullae, pulmonary cysts, and lung cavities. Blebs and bullae can be classified by their wall thickness.