Related Research Articles

The esophagus or oesophagus, non-technically known also as the food pipe or gullet, is an organ in vertebrates through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. The esophagus is a fibromuscular tube, about 25 cm (10 in) long in adults, that travels behind the trachea and heart, passes through the diaphragm, and empties into the uppermost region of the stomach. During swallowing, the epiglottis tilts backwards to prevent food from going down the larynx and lungs. The word oesophagus is from Ancient Greek οἰσοφάγος (oisophágos), from οἴσω (oísō), future form of φέρω + ἔφαγον.

Dysphagia is difficulty in swallowing. Although classified under "symptoms and signs" in ICD-10, in some contexts it is classified as a condition in its own right.
Swallowing, sometimes called deglutition in scientific contexts, is the process in the human or animal body that allows for a substance to pass from the mouth, to the pharynx, and into the esophagus, while shutting the epiglottis. Swallowing is an important part of eating and drinking. If the process fails and the material goes through the trachea, then choking or pulmonary aspiration can occur. In the human body the automatic temporary closing of the epiglottis is controlled by the swallowing reflex.

Pulmonary aspiration is the entry of material such as pharyngeal secretions, food or drink, or stomach contents from the oropharynx or gastrointestinal tract, into the larynx and lower respiratory tract, the portions of the respiratory system from the trachea (windpipe) to the lungs. A person may inhale the material, or it may be delivered into the tracheobronchial tree during positive pressure ventilation. When pulmonary aspiration occurs during eating and drinking, the aspirated material is often colloquially referred to as "going down the wrong pipe."

The epiglottis is a leaf-shaped flap in the throat that prevents food and water from entering the windpipe and the lungs. It stays open during breathing, allowing air into the larynx. During swallowing, it closes to prevent aspiration of food into the lungs, forcing the swallowed liquids or food to go along the esophagus toward the stomach instead. It is thus the valve that diverts passage to either the trachea or the esophagus.
The pharyngeal reflex or gag reflex is a reflex muscular contraction of the back of the throat, evoked by touching the roof of the mouth, the back of the tongue, the area around the tonsils, the uvula, and the back of the throat. It, along with other aerodigestive reflexes such as reflexive pharyngeal swallowing, prevents objects in the oral cavity from entering the throat except as part of normal swallowing and helps prevent choking, and is a form of coughing. The pharyngeal reflex is different from the laryngeal spasm, which is a reflex muscular contraction of the vocal cords.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).

Respiratory arrest is caused by apnea or respiratory dysfunction severe enough it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may damage vital organs especially the brain, possibly permanently. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.
A Zenker's diverticulum, also pharyngeal pouch, is a diverticulum of the mucosa of the human pharynx, just above the cricopharyngeal muscle. It is a pseudo diverticulum.

Plummer–Vinson syndrome is a rare disease characterized by difficulty swallowing, iron-deficiency anemia, glossitis, cheilosis and esophageal webs. Treatment with iron supplementation and mechanical widening of the esophagus generally provides an excellent outcome.

Aspiration pneumonia is a type of lung infection that is due to a relatively large amount of material from the stomach or mouth entering the lungs. Signs and symptoms often include fever and cough of relatively rapid onset. Complications may include lung abscess. Some include chemical induced inflammation of the lungs as a subtype, which occurs from acidic but non-infectious stomach contents entering the lungs.
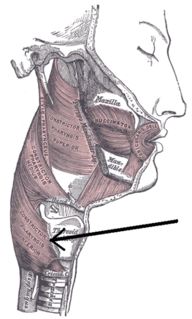
The inferior pharyngeal constrictor muscle is a skeletal muscle of the neck. It is the thickest of the three outer pharyngeal muscles. It arises from the sides of the cricoid cartilage and the thyroid cartilage. It is supplied by the vagus nerve. It is active during swallowing, and partially during breathing and speech. It may be affected by Zenker's diverticulum.
Oropharyngeal dysphagia arises from abnormalities of muscles, nerves or structures of the oral cavity, pharynx, and upper esophageal sphincter.
Esophageal dysphagia is a form of dysphagia where the underlying cause arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach, usually due to mechanical causes or motility problems.
Baby-led weaning is an approach to adding complementary foods to a baby's diet of breast milk or formula. BLW facilitates oral motor development and strongly focuses on the family meal, while maintaining eating as a positive, interactive experience. Baby-led weaning allows babies to control their solid food consumption by "self-feeding" from the start of their experience with food. The term weaning does not imply giving up breast milk or formula, but simply indicates the introduction of foods other than breast milk or formula.

Nutcracker esophagus, or hypertensive peristalsis, is a disorder of the movement of the esophagus characterized by contractions in the smooth muscle of the esophagus in a normal sequence but at an excessive amplitude or duration. Nutcracker esophagus is one of several motility disorders of the esophagus, including achalasia and diffuse esophageal spasm. It causes difficulty swallowing, or dysphagia, to both solid and liquid foods, and can cause significant chest pain; it may also be asymptomatic. Nutcracker esophagus can affect people of any age but is more common in the sixth and seventh decades of life.

Aphagia is the inability or refusal to swallow. The word is derived from the Ancient Greek prefix α, meaning "not" or "without," and the suffix φαγία, derived from the verb φαγεῖν, meaning "to eat." It is related to dysphagia which is difficulty swallowing, and odynophagia, painful swallowing. Aphagia may be temporary or long term, depending on the affected organ. It is an extreme, life-threatening case of dysphagia. Depending on the cause, untreated dysphagia may develop into aphagia.

The pharynx is the part of the throat behind the mouth and nasal cavity, and above the oesophagus and trachea. It is found in vertebrates and invertebrates, though its structure varies across species. The pharynx carries food and air to the esophagus and larynx respectively. The flap of cartilage called the epiglottis stops food from entering the larynx.
Flexible Endoscopic Evaluation of Swallowing with Sensory Testing (FEESST), or laryngopharyngeal sensory testing, is a technique used to directly examine motor and sensory functions of swallowing so that proper treatment can be given to patients with swallowing difficulties to decrease their risk of aspiration and choking. FEESST was invented by Dr. Jonathan E. Aviv MD, FACS in 1993, and has been used by otolaryngologists, pulmonologists, gastroenterologists, intensivists and speech-language pathologists for the past 20 years.

Advanced airway management is the subset of airway management that involves advanced training, skill, and invasiveness. It encompasses various techniques performed to create an open or patent airway – a clear path between a patient's lungs and the outside world.
References
- 1 2 3 4 Robbins JA, Hamilton JW, Lof GL, Kempster G. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology 1992;103:823-9.
- 1 2 3 Tracy F, Logemann JA, Kahrilas PJ, Jacob P, Kobara M, Krugla C. Preliminary observations on the effects of age on oropharyngeal deglutition. Dysphagia 1989;4:90-4.
- 1 2 Shaw DW, Cook IJ, Dent J et al. Age influences oropharyngeal and upper esophageal sphincter function during swallowing. Gastroenterology 1990;98:A390.
- 1 2 3 Shaw DW, Cook IJ, Gabb M et al. Influence of normal aging on oropharyngeal and upper esophageal sphincter function during swallow. Am J Physiol 1995;L68:G389-G390.
- 1 2 Robbins J, Coyle J, Roecker E, Rosenbek J, Wood J. Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia 1999;14:228-32.
- 1 2 Robbins J, Levine R, Wood J, Roecker E, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol Med Sci 1995;50:M257-M262.
- 1 2 Nicosia MA, Hind JA, Roecker EB, Carnes M, Robbins JA. Age effects on the temporal evolution of isometric and swallowing pressure. J Gerontol Med Sci 2000;55A:M634-M640.