Related Research Articles

Lemierre's syndrome is infectious thrombophlebitis of the internal jugular vein. It most often develops as a complication of a bacterial sore throat infection in young, otherwise healthy adults. The thrombophlebitis is a serious condition and may lead to further systemic complications such as bacteria in the blood or septic emboli.

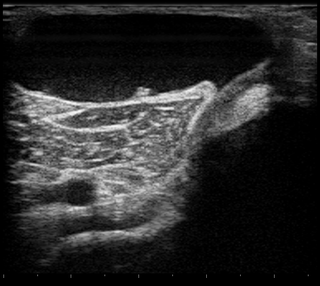
Medical ultrasound includes diagnostic techniques using ultrasound, as well as therapeutic applications of ultrasound. In diagnosis, it is used to create an image of internal body structures such as tendons, muscles, joints, blood vessels, and internal organs, to measure some characteristics or to generate an informative audible sound. The usage of ultrasound to produce visual images for medicine is called medical ultrasonography or simply sonography, or echography. The practice of examining pregnant women using ultrasound is called obstetric ultrasonography, and was an early development of clinical ultrasonography. The machine used is called an ultrasound machine, a sonograph or an echograph. The visual image formed using this technique is called an ultrasonogram, a sonogram or an echogram.

Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.
A Baker's cyst, also known as a popliteal cyst, is a type of fluid collection behind the knee. Often there are no symptoms. If symptoms do occur these may include swelling and pain behind the knee, or knee stiffness. If the cyst breaks open, pain may significantly increase with swelling of the calf. Rarely complications such as deep vein thrombosis, peripheral neuropathy, ischemia, or compartment syndrome may occur.
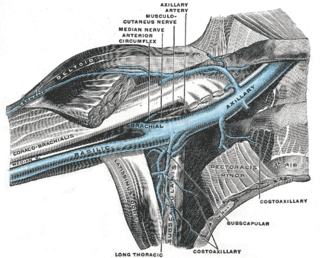
Paget–Schroetter disease is a form of upper extremity deep vein thrombosis (DVT), a medical condition in which blood clots form in the deep veins of the arms. These DVTs typically occur in the axillary and/or subclavian veins.
In medicine, Homans' sign is considered by some physicians to be a sign of deep vein thrombosis (DVT). It was defined by John Homans in 1941 as discomfort behind the knee upon forced dorsiflexion of the foot. After many examples of false-positive Homans' signs were reported, Homans redefined it in 1944, stating that "discomfort need have no part in the reaction", and that increased resistance, involuntary flexure of the knee or pain in the calf upon forced dorsiflexion should be considered positive responses.

Renal vein thrombosis (RVT) is the formation of a clot in the vein that drains blood from the kidneys, ultimately leading to a reduction in the drainage of one or both kidneys and the possible migration of the clot to other parts of the body. First described by German pathologist Friedrich Daniel von Recklinghausen in 1861, RVT most commonly affects two subpopulations: newly born infants with blood clotting abnormalities or dehydration and adults with nephrotic syndrome.

May–Thurner syndrome (MTS), also known as the iliac vein compression syndrome, is a condition in which compression of the common venous outflow tract of the left lower extremity may cause discomfort, swelling, pain or iliofemoral deep vein thrombosis.

Vascular disease is a class of diseases of the vessels of the circulatory system in the body, including blood vessels – the arteries and veins, and the lymphatic vessels. Vascular disease is a subgroup of cardiovascular disease. Disorders in this vast network of blood and lymph vessels can cause a range of health problems that can sometimes become severe, and fatal. Coronary heart disease for example, is the leading cause of death for men and women in the United States.

Venography is a procedure in which an X-ray of the veins, a venogram, is taken after a special dye is injected into the bone marrow or veins. The dye has to be injected constantly via a catheter, making it an invasive procedure. Normally the catheter is inserted by the groin and moved to the appropriate site by navigating through the vascular system.
The term venous translucence has been used in phlebology since 1996 by surgeon Pedro Fernandes Neto during ambulatory clinical exams in Brazil. His results were published in the annals of the national and international congresses of angiology. Venous translucence is the process of reflective image visualization of veins by light, which reaches up to the superficial venous system. It is a non-invasive method. Since it is a simple, low-cost technique it can be repeated as needed, which is useful in disease-process monitoring. It is a new diagnostic procedure, still undergoing investigation; more analysis is necessary to hone its technical aspects. Venous translucence is based on optical physics. It is caused by the refraction, absorption and reflection of light. The color which is not absorbed is reflected, and is the one that is seen. Therefore, venous translumination is based on the incidence of luminosity on the vein, where part of the light is absorbed and another reflected.
Emergency ultrasound employing point-of-care ultrasound (POCUS) is the application of ultrasound at the point of care to make immediate patient-care decisions. It is performed by the health care professional caring for the injured or ill persons. This point-of-care use of ultrasound is often to evaluate an emergency medical condition, in settings such as an emergency department, critical care unit, ambulance, or combat zone.

Chronic venous insufficiency (CVI) is a medical condition in which blood pools in the veins, straining the walls of the vein. The most common cause of CVI is superficial venous reflux which is a treatable condition. As functional venous valves are required to provide for efficient blood return from the lower extremities, this condition typically affects the legs. If the impaired vein function causes significant symptoms, such as swelling and ulcer formation, it is referred to as chronic venous disease. It is sometimes called chronic peripheral venous insufficiency and should not be confused with post-thrombotic syndrome in which the deep veins have been damaged by previous deep vein thrombosis.
Phlegmasia alba dolens is part of a spectrum of diseases related to deep vein thrombosis. Historically, it was commonly seen during pregnancy and in mothers who have just given birth. In cases of pregnancy, it is most often seen during the third trimester, resulting from a compression of the left common iliac vein against the pelvic rim by the enlarged uterus. Today, this disease is most commonly related to some form of underlying malignancy. Hypercoagulability is a well-known state that occurs in many cancer states. The incidence of this disease is not well reported.

Superficial thrombophlebitis is a thrombosis and inflammation of superficial veins presenting as a painful induration (thickening) with erythema, often in a linear or branching configuration with a cordlike appearance.
Septic thrombophlebitis is characterized by a bacterial or fungal infection that coexists with venous thrombosis. Deep veins or superficial veins could be affected. Septic thrombophlebitis can manifest as anything from a harmless condition that affects a small area of superficial veins to serious systemic infections that cause shock and even death.

Superficial vein thrombosis (SVT) is a blood clot formed in a superficial vein, a vein near the surface of the body. Usually there is thrombophlebitis, which is an inflammatory reaction around a thrombosed vein, presenting as a painful induration with redness. SVT itself has limited significance when compared to a deep vein thrombosis (DVT), which occurs deeper in the body at the deep venous system level. However, SVT can lead to serious complications, and is therefore no longer regarded as a benign condition. If the blood clot is too near the saphenofemoral junction there is a higher risk of pulmonary embolism, a potentially life-threatening complication.

Ultrasonography of suspected or previously confirmed chronic venous insufficiency of leg veins is a risk-free, non-invasive procedure. It gives information about the anatomy, physiology and pathology of mainly superficial veins. As with heart ultrasound (echocardiography) studies, venous ultrasonography requires an understanding of hemodynamics in order to give useful examination reports. In chronic venous insufficiency, sonographic examination is of most benefit; in confirming varicose disease, making an assessment of the hemodynamics, and charting the progression of the disease and its response to treatment. It has become the reference standard for examining the condition and hemodynamics of the lower limb veins. Particular veins of the deep venous system (DVS), and the superficial venous system (SVS) are looked at. The great saphenous vein (GSV), and the small saphenous vein (SSV) are superficial veins which drain into respectively, the common femoral vein and the popliteal vein. These veins are deep veins. Perforator veins drain superficial veins into the deep veins. Three anatomic compartments are described, (N1) containing the deep veins, (N2) containing the perforator veins, and (N3) containing the superficial veins, known as the saphenous compartment. This compartmentalisation makes it easier for the examiner to systematize and map. The GSV can be located in the saphenous compartment where together with the Giacomini vein and the accessory saphenous vein (ASV) an image resembling an eye, known as the 'eye sign' can be seen. The ASV which is often responsible for varicose veins, can be located at the 'alignment sign', where it is seen to align with the femoral vessels.

Ultrasonography in suspected deep vein thrombosis focuses primarily on the femoral vein and the popliteal vein, because thrombi in these veins are associated with the greatest risk of harmful pulmonary embolism.
References
- ↑ 1. Munk, Peter L Lee, Mark J. Ruptured Baker's cyst producing a pseudothrombophlebitis syndrome Canadian Journal of Surgery Aug 2000 43(4) 255
- ↑ Drescher MJ. Smally AJ. Thrombophlebitis and pseudothrombophlebitis in the ED. Am J Emerg Med. 15(7):683-5, 1997 Nov.
- ↑ Drescher MJ. Smally AJ. Thrombophlebitis and pseudothrombophlebitis in the ED. Am J Emerg Med. 15(7):683-5, 1997 Nov.