Related Research Articles

A head injury is any injury that results in trauma to the skull or brain. The terms traumatic brain injury and head injury are often used interchangeably in the medical literature. Because head injuries cover such a broad scope of injuries, there are many causes—including accidents, falls, physical assault, or traffic accidents—that can cause head injuries.

An intracranial aneurysm, also known as a cerebral aneurysm, is a cerebrovascular disorder in which weakness in the wall of a cerebral artery or vein causes a localized dilation or ballooning of the blood vessel.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, death.

Stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functioning properly.

Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consciousness, fever, weakness, numbness, and sometimes seizures. Neck stiffness or neck pain are also relatively common. In about a quarter of people a small bleed with resolving symptoms occurs within a month of a larger bleed.
A thunderclap headache is a headache that is severe and has a sudden onset. It is defined as a severe headache that takes seconds to minutes to reach maximum intensity. Although approximately 75% are attributed to "primary" headaches—headache disorder, non-specific headache, idiopathic thunderclap headache, or uncertain headache disorder—the remainder are secondary to other causes, which can include some extremely dangerous acute conditions, as well as infections and other conditions. Usually, further investigations are performed to identify the underlying cause.

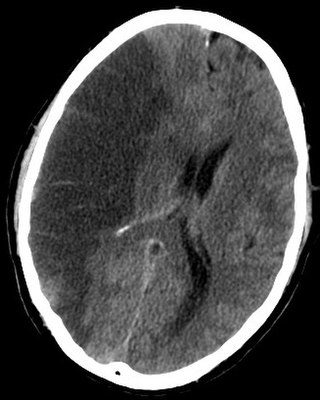
Intracerebral hemorrhage (ICH), also known as cerebral bleed, intraparenchymal bleed, and haemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is one kind of bleeding within the skull and one kind of stroke. Symptoms can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, and neck stiffness. Often, symptoms get worse over time. Fever is also common.
Brain ischemia is a condition in which there is insufficient bloodflow to the brain to meet metabolic demand. This leads to poor oxygen supply or cerebral hypoxia and thus leads to the death of brain tissue or cerebral infarction/ischemic stroke. It is a sub-type of stroke along with subarachnoid hemorrhage and intracerebral hemorrhage.

Vertebral artery dissection (VAD) is a flap-like tear of the inner lining of the vertebral artery, which is located in the neck and supplies blood to the brain. After the tear, blood enters the arterial wall and forms a blood clot, thickening the artery wall and often impeding blood flow. The symptoms of vertebral artery dissection include head and neck pain and intermittent or permanent stroke symptoms such as difficulty speaking, impaired coordination, and visual loss. It is usually diagnosed with a contrast-enhanced CT or MRI scan.

Intraventricular hemorrhage (IVH), also known as intraventricular bleeding, is a bleeding into the brain's ventricular system, where the cerebrospinal fluid is produced and circulates through towards the subarachnoid space. It can result from physical trauma or from hemorrhagic stroke.

Cerebral venous sinus thrombosis (CVST), cerebral venous and sinus thrombosis or cerebral venous thrombosis (CVT), is the presence of a blood clot in the dural venous sinuses, the cerebral veins, or both. Symptoms may include severe headache, visual symptoms, any of the symptoms of stroke such as weakness of the face and limbs on one side of the body, and seizures, which occur in around 40% of patients.

Neurocritical care is a medical field that treats life-threatening diseases of the nervous system and identifies, prevents, and treats secondary brain injury.

An external ventricular drain (EVD), also known as a ventriculostomy or extraventricular drain, is a device used in neurosurgery to treat hydrocephalus and relieve elevated intracranial pressure when the normal flow of cerebrospinal fluid (CSF) inside the brain is obstructed. An EVD is a flexible plastic catheter placed by a neurosurgeon or neurointensivist and managed by intensive care unit (ICU) physicians and nurses. The purpose of external ventricular drainage is to divert fluid from the ventricles of the brain and allow for monitoring of intracranial pressure. An EVD must be placed in a center with full neurosurgical capabilities, because immediate neurosurgical intervention can be needed if a complication of EVD placement, such as bleeding, is encountered.

Midline shift is a shift of the brain past its center line. The sign may be evident on neuroimaging such as CT scanning. The sign is considered ominous because it is commonly associated with a distortion of the brain stem that can cause serious dysfunction evidenced by abnormal posturing and failure of the pupils to constrict in response to light. Midline shift is often associated with high intracranial pressure (ICP), which can be deadly. In fact, midline shift is a measure of ICP; presence of the former is an indication of the latter. Presence of midline shift is an indication for neurosurgeons to take measures to monitor and control ICP. Immediate surgery may be indicated when there is a midline shift of over 5 mm. The sign can be caused by conditions including traumatic brain injury, stroke, hematoma, or birth deformity that leads to a raised intracranial pressure.
The Neurocritical Care Society (NCS) is an international, multidisciplinary medical society first established in 2002. The Society is dedicated to improving the care and outcomes of patients with life-threatening neurologic illnesses in the intensive care unit. Common illnesses requiring neurocritical care include ischemic stroke, subarachnoid hemorrhage, intracranial hemorrhage, traumatic brain and spinal cord injury, coma, and status epilepticus. Its members are health professionals providing care to critically ill and injured patients. The Society supports research and education, and advocates on issues related to neurointensive care, neurocritical care, and general critical care.
Clinicians routinely check the pupils of critically injured and ill patients to monitor neurological status. However, manual pupil measurements have been shown to be subjective, inaccurate, and not repeatable or consistent. Automated assessment of the pupillary light reflex has emerged as an objective means of measuring pupillary reactivity across a range of neurological diseases, including stroke, traumatic brain injury and edema, tumoral herniation syndromes, and sports or war injuries. Automated pupillometers are used to assess an array of objective pupillary variables including size, constriction velocity, latency, and dilation velocity, which are normalized and standardized to compute an indexed score such as the Neurological Pupil index (NPi).

There is increasing evidence suggesting that COVID-19 causes both acute and chronic neurologicalor psychological symptoms. Caregivers of COVID-19 patients also show a higher than average prevalence of mental health concerns. These symptoms result from multiple different factors.
Stephan A. Mayer is an American neurologist and critical care physician who currently serves as Director of Neurocritical Care and Emergency Neurology Services for the Westchester Medical Center Health System. Mayer is most noted for his research in subarachnoid and intracerebral hemorrhage, acute ischemic stroke, cardiac arrest, coma, status epilepticus, brain multimodality monitoring, therapeutic temperature modulation, and outcomes after severe brain injury. He has gained media attention for popularizing the concept that physicians have historically underestimated the brain’s resilience and capacity for recovery. He has authored over 400 original research publications, 200 chapters and review articles, and 370 abstracts.
Spinal cord stroke is a rare type of stroke with compromised blood flow to any region of spinal cord owing to occlusion or bleeding, leading to irreversible neuronal death. It can be classified into two types, ischaemia and haemorrhage, in which the former accounts for 86% of all cases, a pattern similar to cerebral stroke. The disease is either arisen spontaneously from aortic illnesses or postoperatively. It deprives patients of motor function or sensory function, and sometimes both. Infarction usually occurs in regions perfused by anterior spinal artery, which spans the anterior two-thirds of spinal cord. Preventions of the disease include decreasing the risk factors and maintaining enough spinal cord perfusion pressure during and after the operation. The process of diagnosing the ischemic and hemorrhagic spinal cord stroke includes applying different MRI protocols and CT scan. Treatments for spinal cord stroke are mainly determined by the symptoms and the causes of the disease. For example, antiplatelet and corticosteroids might be used to reduce the risk of blood clots in ischaemic spinal stroke patients, while rapid surgical decompression is applied to minimize neurological injuries in haemorrhagic spinal stroke patients instead. Patients may spend years for rehabilitation after the spinal cord stroke.
References
- ↑ Frontera, Jennifer; Mainali, Shraddha; Fink, Ericka L.; Robertson, Courtney L.; Schober, Michelle; Ziai, Wendy; Menon, David; Kochanek, Patrick M.; Suarez, Jose I.; Helbok, Raimund (August 2020). "Global Consortium Study of Neurological Dysfunction in COVID-19 (GCS-NeuroCOVID): Study Design and Rationale". Neurocritical Care. 33 (1): 25–34. doi:10.1007/s12028-020-00995-3. ISSN 1541-6933. PMC 7243953 . PMID 32445105.
- ↑ McNett, Molly; Fink, Ericka L.; Schober, Michelle; Mainali, Shraddha; Helbok, Raimund; Robertson, Courtney L.; Mejia-Mantilla, Jorge; Kurtz, Pedro; Righy, Cássia; Roa, Juan D.; Villamizar-Rosales, Carlos (December 2020). "The Global Consortium Study of Neurological Dysfunction in COVID-19 (GCS-NeuroCOVID): Development of Case Report Forms for Global Use". Neurocritical Care. 33 (3): 793–828. doi:10.1007/s12028-020-01100-4. ISSN 1541-6933. PMC 7500499 . PMID 32948987.
- ↑ Chou, Sherry H.-Y.; Beghi, Ettore; Helbok, Raimund; Moro, Elena; Sampson, Joshua; Altamirano, Valeria; Mainali, Shraddha; Bassetti, Claudio; Suarez, Jose I.; McNett, Molly (2021-05-11). "Global Incidence of Neurological Manifestations Among Patients Hospitalized With COVID-19—A Report for the GCS-NeuroCOVID Consortium and the ENERGY Consortium". JAMA Network Open. 4 (5): e2112131. doi: 10.1001/jamanetworkopen.2021.12131 . ISSN 2574-3805. PMC 8114143 . PMID 33974053.
- 1 2 3 "Bench AND bedside: winning combination for Sherry Chou : Medicine Focus" . Retrieved 2020-04-21.
- ↑ "Chou, Sherry | Department of Critical Care Medicine". ccm.pitt.edu. Retrieved 2020-04-21.
- ↑ "Critical Care Neurology Research - Brigham and Women's Hospital". www.brighamandwomens.org. Retrieved 2020-04-21.
- ↑ "INCLINE Grant for Neurocritical Care Research Awarded to Sherry Chou, MD, MMSc | Department of Critical Care Medicine". ccm.pitt.edu. Retrieved 2020-04-21.
- ↑ Rabin, Roni Caryn (2020-04-01). "Some Coronavirus Patients Show Signs of Brain Ailments". The New York Times. ISSN 0362-4331 . Retrieved 2020-04-21.
- 1 2 "In Some Cases, COVID-19 May Harm the Brain". WebMD. Retrieved 2020-04-21.
- ↑ Higgs, Robert (2020-04-07). "Medical experts suspect COVID-19 coronavirus capable of harming the brain". cleveland. Retrieved 2020-04-22.
- ↑ "Education and Research". www.aan.com. Retrieved 2020-04-22.
- ↑ Wadman, Meredith; Couzin-Frankel, Jennifer; Kaiser, Jocelyn; Matacic, Catherine (2020-04-17). "How does coronavirus kill? Clinicians trace a ferocious rampage through the body, from brain to toes". AAAS. Retrieved 2020-04-21.
- ↑ "Coronavirus Disease 2019 (COVID-19) – Symptoms". Centers for Disease Control and Prevention. 2020-04-17. Retrieved 2020-04-21.
- ↑ "Doctors investigate rare COVID-19 symptoms in effort to move quickly from anecdotes to science". CBC.ca. 8 April 2020. Retrieved 17 October 2021.
- ↑ "Neurocritical Care Society Inductees". www.neurocriticalcare.org. Retrieved 2020-04-21.
- ↑ Chou, Sherry H.-Y.; Feske, Steven K.; Atherton, Juli; Konigsberg, Rachael G.; De Jager, Philip L.; Du, Rose; Ogilvy, Christopher S.; Lo, Eng H.; Ning, MingMing (2012-10-01). "Early Elevation of Serum Tumor Necrosis Factor-α Is Associated With Poor Outcome in Subarachnoid Hemorrhage". Journal of Investigative Medicine. 60 (7): 1054–1058. doi:10.2310/jim.0b013e3182686932. ISSN 1081-5589. PMC 3740211 . PMID 22918199.
- ↑ Chou, Sherry H.-Y.; Lan, Jing; Esposito, Elga; Ning, MingMing; Balaj, Leonora; Ji, Xunming; Lo, Eng H.; Hayakawa, Kazuhide (August 2017). "Extracellular Mitochondria in Cerebrospinal Fluid and Neurological Recovery After Subarachnoid Hemorrhage". Stroke. 48 (8): 2231–2237. doi:10.1161/strokeaha.117.017758. ISSN 0039-2499. PMC 5526718 . PMID 28663512.
- ↑ Berkowitz, A.L.; Westover, B.; Bianchi, M.T.; Chou, S.H. (2015-03-12). "Aspirin for secondary prevention after stroke of unknown etiology in resource-limited settings: a decision analysis". Annals of Global Health. 81 (1): 87. doi: 10.1016/j.aogh.2015.02.702 . ISSN 2214-9996.
- ↑ Berkowitz, A. L.; Westover, M. B.; Bianchi, M. T.; Chou, S. H.- Y. (2014-07-23). "Aspirin for acute stroke of unknown etiology in resource-limited settings: A decision analysis". Neurology. 83 (9): 787–793. doi:10.1212/wnl.0000000000000730. ISSN 0028-3878. PMC 4155044 . PMID 25056582.
- ↑ "Editorial Board - NCC On Call". oncall.neurocriticalcare.org. Retrieved 2020-04-21.