The adrenal glands are endocrine glands that produce a variety of hormones including adrenaline and the steroids aldosterone and cortisol. They are found above the kidneys. Each gland has an outer cortex which produces steroid hormones and an inner medulla. The adrenal cortex itself is divided into three main zones: the zona glomerulosa, the zona fasciculata and the zona reticularis.
Adrenocorticotropic hormone is a polypeptide tropic hormone produced by and secreted by the anterior pituitary gland. It is also used as a medication and diagnostic agent. ACTH is an important component of the hypothalamic-pituitary-adrenal axis and is often produced in response to biological stress. Its principal effects are increased production and release of cortisol and androgens by the zona fasiculata and zona reticularis, respectively. ACTH is also related to the circadian rhythm in many organisms.

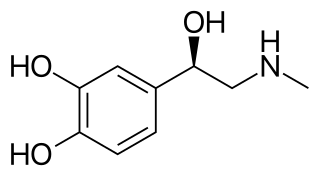
A catecholamine is a monoamine neurotransmitter, an organic compound that has a catechol and a side-chain amine.

Stress, whether physiological, biological or psychological, is an organism's response to a stressor such as an environmental condition. When stressed by stimuli that alter an organism's environment, multiple systems respond across the body. In humans and most mammals, the autonomic nervous system and hypothalamic-pituitary-adrenal (HPA) axis are the two major systems that respond to stress. Two well-known hormones that humans produce during stressful situations are adrenaline and cortisol.

The hypothalamic–pituitary–adrenal axis is a complex set of direct influences and feedback interactions among three components: the hypothalamus, the pituitary gland, and the adrenal glands. These organs and their interactions constitute the HPS axis.
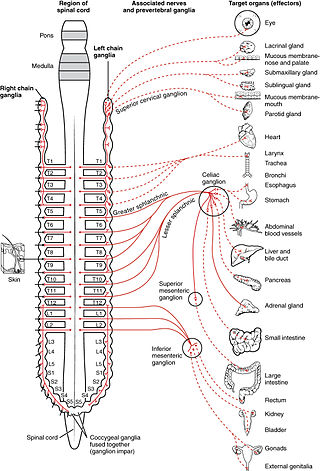
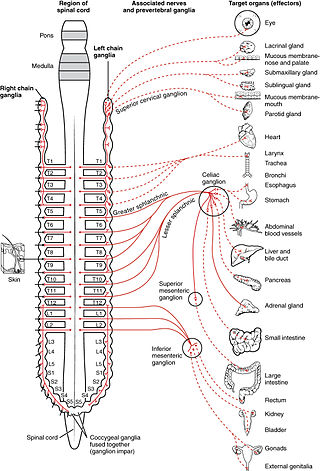
The sympathetic nervous system is one of the three divisions of the autonomic nervous system, the others being the parasympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.

Cortisol is a steroid hormone in the glucocorticoid class of hormones and a stress hormone. When used as medication, it is known as hydrocortisone.

The fight-or-flight or the fight-flight-freeze-or-fawn is a physiological reaction that occurs in response to a perceived harmful event, attack, or threat to survival. It was first described by Walter Bradford Cannon in 1915. His theory states that animals react to threats with a general discharge of the sympathetic nervous system, preparing the animal for fighting or fleeing. More specifically, the adrenal medulla produces a hormonal cascade that results in the secretion of catecholamines, especially norepinephrine and epinephrine. The hormones estrogen, testosterone, and cortisol, as well as the neurotransmitters dopamine and serotonin, also affect how organisms react to stress. The hormone osteocalcin might also play a part.

The adrenal medulla is the inner part of the adrenal gland. It is located at the center of the gland, being surrounded by the adrenal cortex. It is the innermost part of the adrenal gland, consisting of chromaffin cells that secrete catecholamines, including epinephrine (adrenaline), norepinephrine (noradrenaline), and a small amount of dopamine, in response to stimulation by sympathetic preganglionic neurons.

Chromaffin cells, also called pheochromocytes, are neuroendocrine cells found mostly in the medulla of the adrenal glands in mammals. These cells serve a variety of functions such as serving as a response to stress, monitoring carbon dioxide and oxygen concentrations in the body, maintenance of respiration and the regulation of blood pressure. They are in close proximity to pre-synaptic sympathetic ganglia of the sympathetic nervous system, with which they communicate, and structurally they are similar to post-synaptic sympathetic neurons. In order to activate chromaffin cells, the splanchnic nerve of the sympathetic nervous system releases acetylcholine, which then binds to nicotinic acetylcholine receptors on the adrenal medulla. This causes the release of catecholamines. The chromaffin cells release catecholamines: ~80% of adrenaline (epinephrine) and ~20% of noradrenaline (norepinephrine) into systemic circulation for systemic effects on multiple organs, and can also send paracrine signals. Hence they are called neuroendocrine cells.

The baroreflex or baroreceptor reflex is one of the body's homeostatic mechanisms that helps to maintain blood pressure at nearly constant levels. The baroreflex provides a rapid negative feedback loop in which an elevated blood pressure causes the heart rate to decrease. Decreased blood pressure decreases baroreflex activation and causes heart rate to increase and to restore blood pressure levels. Their function is to sense pressure changes by responding to change in the tension of the arterial wall. The baroreflex can begin to act in less than the duration of a cardiac cycle and thus baroreflex adjustments are key factors in dealing with postural hypotension, the tendency for blood pressure to decrease on standing due to gravity.
Acute stress reaction (ASR), also known as psychological shock, mental shock, or simply shock, and acute stress disorder (ASD), is a psychological response to a terrifying, traumatic, or surprising experience. Combat stress reaction (CSR) is a similar response to the trauma of war. The reactions may include but are not limited to intrusive or dissociative symptoms, and reactivity symptoms such as avoidance or arousal. It may be exhibited for days or weeks after the traumatic event. If the condition is not correctly addressed, it may develop into post-traumatic stress disorder (PTSD).
Secondary hypertension is a type of hypertension which has a specific and identifiable underlying primary cause. It is much less common than essential hypertension, affecting only 5-10% of hypertensive patients. It has many different causes including obstructive sleep apnea, kidney disease, endocrine diseases, and tumors. The cause of secondary hypertension varies significantly with age. It also can be a side effect of many medications.
In humans and other animals, the adrenocortical hormones are hormones produced by the adrenal cortex, the outer region of the adrenal gland. These polycyclic steroid hormones have a variety of roles that are crucial for the body's response to stress, and they also regulate other functions in the body. Threats to homeostasis, such as injury, chemical imbalances, infection, or psychological stress, can initiate a stress response. Examples of adrenocortical hormones that are involved in the stress response are aldosterone and cortisol. These hormones also function in regulating the conservation of water by the kidneys and glucose metabolism, respectively.

In the autonomic nervous system, nerve fibers from the ganglion to the effector organ are called postganglionic nerve fibers.

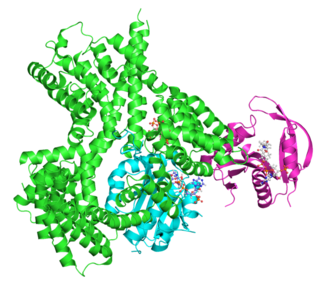
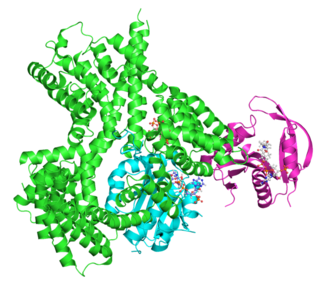
Phenylethanolamine N-methyltransferase (PNMT) is an enzyme found primarily in the adrenal medulla that converts norepinephrine (noradrenaline) to epinephrine (adrenaline). It is also expressed in small groups of neurons in the human brain and in selected populations of cardiomyocytes.

Norepinephrine (NE), also called noradrenaline (NA) or noradrenalin, is an organic chemical in the catecholamine family that functions in the brain and body as a hormone, neurotransmitter and neuromodulator. The name "noradrenaline" is more commonly used in the United Kingdom, whereas "norepinephrine" is usually preferred in the United States. "Norepinephrine" is also the international nonproprietary name given to the drug. Regardless of which name is used for the substance itself, parts of the body that produce or are affected by it are referred to as noradrenergic.
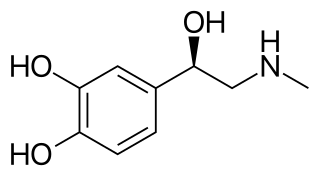
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions. It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands and by a small number of neurons in the medulla oblongata. It plays an essential role in the fight-or-flight response by increasing blood flow to muscles, heart output by acting on the SA node, pupil dilation response, and blood sugar level. It does this by binding to alpha and beta receptors. It is found in many animals, including humans, and some single-celled organisms. It has also been isolated from the plant Scoparia dulcis found in Northern Vietnam.
Non-tropic hormones are hormones that directly stimulate target cells to induce effects. This differs from the tropic hormones, which act on another endocrine gland. Non-tropic hormones are those that act directly on targeted tissues or cells, and not on other endocrine gland to stimulate release of other hormones. Many hormones act in a chain reaction. Tropic hormones usually act in the beginning of the reaction stimulating other endocrine gland to eventually release non-tropic hormones. These are the ones that act in the end of the chain reaction on other cells that are not part of other endocrine gland. The Hypothalamic-pituitary-adrenal axis is a perfect example of this chain reaction. The reaction begins in the hypothalamus with a release of corticotropin-releasing hormone/factor. This stimulates the anterior pituitary and causes it to release Adrenocorticotropic hormone to the adrenal glands. Lastly, cortisol (non-tropic) is secreted from the adrenal glands and goes into the bloodstream where it can have more widespread effects on organs and tissues. Since cortisol is what finally reaches other tissues in the body, it is a non-tropic hormone. CRH and ACTH are tropic hormones because they act on the anterior pituitary gland and adrenal glands, respectively, both of which are endocrine glands. Non-tropic hormones are thus often the last piece of a larger process and chain of hormone secretion. Both tropic and non-tropic hormones are necessary for proper endocrine function. For example, if ACTH is inhibited, cortisol can no longer be released because the chain reaction has been interrupted. Some examples of non-tropic hormones are:
Neurocardiology is the study of the neurophysiological, neurological and neuroanatomical aspects of cardiology, including especially the neurological origins of cardiac disorders. The effects of stress on the heart are studied in terms of the heart's interactions with both the peripheral nervous system and the central nervous system.