Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.
Local anesthesia is any technique to induce the absence of sensation in a specific part of the body, generally for the aim of inducing local analgesia, i.e. local insensitivity to pain, although other local senses may be affected as well. It allows patients to undergo surgical and dental procedures with reduced pain and distress. In many situations, such as cesarean section, it is safer and therefore superior to general anesthesia.

A local anesthetic (LA) is a medication that causes absence of all sensation in a specific body part without loss of consciousness, as opposed to a general anesthetic, which eliminates all sensation in the entire body and causes unconsciousness. Local anesthetics are most commonly used to eliminate pain during or after surgery. When it is used on specific nerve pathways, paralysis also can be induced.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory of the experience, it is also possible for victims to have awareness with explicit recall, where they can remember the events related to their surgery.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.
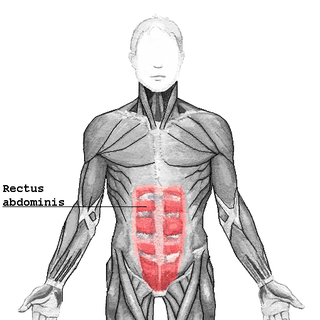
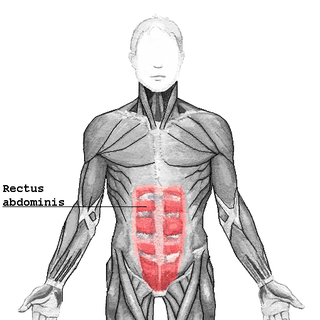
The rectus abdominis muscle, also known as the "abdominal muscle" or simply the "abs", is a pair of segmented skeletal muscle on the ventral aspect of a person's abdomen. The paired muscles are separated at the midline by a band of dense connective tissue called the linea alba, and the connective tissue defining each lateral margin of the rectus abdominus is the linea semilunaris. The muscle extends from the pubic symphysis, pubic crest and pubic tubercle inferiorly, to the xiphoid process and costal cartilages of the 5th-7th ribs superiorly.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.
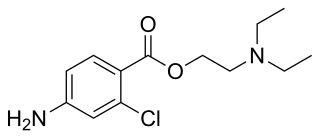
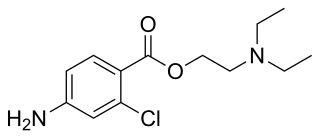
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.

The triangle of auscultation is a relative thinning of the musculature of the back, situated along the medial border of the scapula which allows for improved listening to the lungs.
Dental anesthesia is the application of anesthesia to dentistry. It includes local anesthetics, sedation, and general anesthesia.
Guedel's classification is a means of assessing of depth of general anesthesia introduced by Arthur Ernest Guedel (1883-1956) in 1920.
Continuous wound infiltration (CWI) refers to the continuous infiltration of a local anesthetic into a surgical wound to aid in pain management during post-operative recovery.

Brachial plexus block is a regional anesthesia technique that is sometimes employed as an alternative or as an adjunct to general anesthesia for surgery of the upper extremity. This technique involves the injection of local anesthetic agents in close proximity to the brachial plexus, temporarily blocking the sensation and ability to move the upper extremity. The subject can remain awake during the ensuing surgical procedure, or they can be sedated or even fully anesthetized if necessary.

Intravenous regional anesthesia (IVRA) or Bier's block anesthesia is an anesthetic technique on the body's extremities where a local anesthetic is injected intravenously and isolated from circulation in a target area. The technique usually involves exsanguination of the target region, which forces blood out of the extremity, followed by the application of pneumatic tourniquets to safely stop blood flow. The anesthetic agent is intravenously introduced into the limb and allowed to diffuse into the surrounding tissue while tourniquets retain the agent within the desired area.
The history of neuraxial anesthesia goes back to 1885.

Intercostal nerve block is a nerve block which temporarily or permanently interrupts the flow of signals along an intercostal nerve, usually performed to relieve pain.
Fascia iliaca blocks is a local anesthetic nerve block, a type of regional anesthesia technique, used to provide analgesia or anaesthesia to the hip and thigh. FICB can performed by using ultrasound or with a loss of resistance technique, the latter sometimes referred to as the "two-pop-method". FICB works by affecting the femoral, obturator and the lateral cutaneous nerves with a local anesthetic.

Caudal anaesthesia is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults it is used for chronic low back pain management.