Related Research Articles
An antiseptic is an antimicrobial substance or compound that is applied to living tissue to reduce the possibility of sepsis, infection or putrefaction. Antiseptics are generally distinguished from antibiotics by the latter's ability to safely destroy bacteria within the body, and from disinfectants, which destroy microorganisms found on non-living objects.

An ulcer is a sore on the skin or a mucous membrane, accompanied by the disintegration of tissue. Ulcers can result in complete loss of the epidermis and often portions of the dermis and even subcutaneous fat. Ulcers are most common on the skin of the lower extremities and in the gastrointestinal tract. An ulcer that appears on the skin is often visible as an inflamed tissue with an area of reddened skin. A skin ulcer is often visible in the event of exposure to heat or cold, irritation, or a problem with blood circulation.
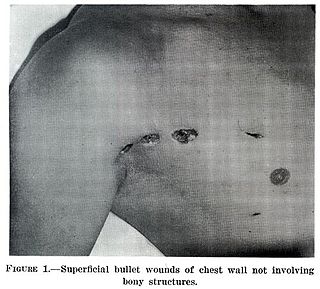
A wound is a rapid onset of injury that involves lacerated or punctured skin, or a contusion from blunt force trauma or compression. In pathology, a wound is an acute injury that damages the epidermis of the skin. To heal a wound, the body undertakes a series of actions collectively known as the wound healing process.

Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.

Pressure ulcers, also known as pressure sores, bed sores or pressure injuries, are localised damage to the skin and/or underlying tissue that usually occur over a bony prominence as a result of usually long-term pressure, or pressure in combination with shear or friction. The most common sites are the skin overlying the sacrum, coccyx, heels, and hips, though other sites can be affected, such as the elbows, knees, ankles, back of shoulders, or the back of the cranium.

Lipedema is a medical condition that is almost exclusively found in women and results in enlargement of both legs due to deposits of fat under the skin. Women of any weight may develop lipedema and the fat associated with lipedema is resistant to traditional weight-loss methods. There is no cure and typically it gets worse over time, pain may be present, and patients bruise easily. Over time mobility may be reduced, and due to reduced quality of life, patients often experience depression. In severe cases the trunk and upper body may be involved. Lipedema is commonly misdiagnosed.

Maggot therapy is a type of biotherapy involving the introduction of live, disinfected maggots into non-healing skin and soft-tissue wounds of a human or other animal for the purpose of cleaning out the necrotic (dead) tissue within a wound (debridement), and disinfection.

Onycholysis is a common medical condition characterized by the painless detachment of the nail from the nail bed, usually starting at the tip and/or sides. On the hands, it occurs particularly on the ring finger but can occur on any of the fingernails. It may also happen to toenails.

Venous ulcer is defined by the American Venous Forum as "a full-thickness defect of skin, most frequently in the ankle region, that fails to heal spontaneously and is sustained by chronic venous disease, based on venous duplex ultrasound testing." Venous ulcers are wounds that are thought to occur due to improper functioning of venous valves, usually of the legs. They are an important cause of chronic wounds, affecting 1% of the population. Venous ulcers develop mostly along the medial distal leg, and can be painful with negative effects on quality of life.
A chronic wound is a wound that does not heal in an orderly set of stages and in a predictable amount of time the way most wounds do; wounds that do not heal within three months are often considered chronic. Chronic wounds seem to be detained in one or more of the phases of wound healing. For example, chronic wounds often remain in the inflammatory stage for too long. To overcome that stage and jump-start the healing process, a number of factors need to be addressed such as bacterial burden, necrotic tissue, and moisture balance of the whole wound. In acute wounds, there is a precise balance between production and degradation of molecules such as collagen; in chronic wounds this balance is lost and degradation plays too large a role.
The history of wound care spans from prehistory to modern medicine. Wounds naturally heal by themselves, but hunter-gatherers would have noticed several factors and certain herbal remedies would speed up or assist the process, especially if it was grievous. In ancient history, this was followed by the realisation of the necessity of hygiene and the halting of bleeding, where wound dressing techniques and surgery developed. Eventually the germ theory of disease also assisted in improving wound care.

Negative-pressure wound therapy (NPWT), also known as a vacuum assisted closure (VAC), is a therapeutic technique using a suction pump, tubing, and a dressing to remove excess exudate and promote healing in acute or chronic wounds and second- and third-degree burns. The therapy involves the controlled application of sub-atmospheric pressure to the local wound environment using a sealed wound dressing connected to a vacuum pump. The use of this technique in wound management started in the 1990s and this technique is often recommended for treatment of a range of wounds including dehisced surgical wounds, closed surgical wounds, open abdominal wounds, open fractures, pressure injuries or pressure ulcers, diabetic foot ulcers, venous insufficiency ulcers, some types of skin grafts, burns, sternal wounds. It may also be considered after a clean surgery in a person who is obese.

Calciphylaxis, also known as calcific uremic arteriolopathy (CUA) or “Grey Scale”, is a rare syndrome characterized by painful skin lesions. The pathogenesis of calciphylaxis is unclear but believed to involve calcification of the small blood vessels located within the fatty tissue and deeper layers of the skin, blood clots, and eventual death of skin cells due to lack of blood flow. It is seen mostly in people with end-stage kidney disease but can occur in the earlier stages of chronic kidney disease and rarely in people with normally functioning kidneys. Calciphylaxis is a rare but serious disease, believed to affect 1-4% of all dialysis patients. It results in chronic non-healing wounds and indicates poor prognosis, with typical life expectancy of less than one year.

An open fracture, also called a compound fracture, is a type of bone fracture that has an open wound in the skin near the fractured bone. The skin wound is usually caused by the bone breaking through the surface of the skin. Open fractures are emergencies and are often caused by high energy trauma such as road traffic accidents and are associated with a high degree of damage to the bone and nearby soft tissue. An open fracture can be life threatening or limb-threatening due to the risk of a deep infection and/or bleeding. Other complications including a risk of malunion of the bone or nonunion of the bone. The severity of open fractures can vary. For diagnosing and classifying open fractures, Gustilo-Anderson open fracture classification is the most commonly used method. It can also be used to guide treatment, and to predict clinical outcomes. Advanced trauma life support is the first line of action in dealing with open fractures and to rule out other life-threatening condition in cases of trauma. The person is also administered antibiotics for at least 24 hours to reduce the risk of an infection. Cephalosporins are generally the first line of antibiotics. Therapeutic irrigation, wound debridement, early wound closure and bone fixation are the main management of open fractures. All these actions aimed to reduce the risk of infections. The bone that is most commonly injured is the tibia and working-age young men are the group of people who are at highest risk of an open fracture. Older people with osteoporosis and soft-tissue problems are also at risk.

Arterial insufficiency ulcers are mostly located on the lateral surface of the ankle or the distal digits. They are commonly caused by peripheral artery disease (PAD).
Transdermal Continuous Oxygen Therapy is a wound closure technique for chronic and acute wounds which blankets a wound in oxygen on a 24-hour basis until the wound heals. Unlike hyperbaric oxygen treatment for chronic wounds, oxygen treatment used in this therapy is not systemic in nature and treats only the wound area. This treatment differs from topical oxygen treatments, as topical oxygen typically involves sporadic treatments of 1–3 hours several times per week, while TCOT treatment is 24/7 by nature.
Wound bed preparation (WBP) is a systematic approach to wound management by identifying and removing barriers to healing. The concept was originally developed in plastic surgery. During the year 2000, the concept was applied to systematizing the treatment of chronic wounds. The 2000 proposals recommended that wound management address the identifiable impediments to healing in order to achieve more successful outcomes. Three publications appeared that year that focused on the concept of managing the healing processes of a wound exudate, bioburden and devitalized tissue. Initially, emphasis was placed on debridement, moisture balance and bacterial balance as the three guiding principles of good wound care, while at the same time recognizing that the provision of care includes a vast array of patient, clinical and environmental variables.
Chronic wound pain is a condition described as unremitting, disabling, and recalcitrant pain experienced by individuals with various types of chronic wounds. Chronic wounds such as venous leg ulcers, arterial ulcers, diabetic foot ulcers, pressure ulcers, and malignant wounds can have an enormous impact on an individual’s quality of life with pain being one of the most distressing symptoms.

Diabetic foot ulcer is a breakdown of the skin and sometimes deeper tissues of the foot that leads to sore formation. It may occur due to a variety of mechanisms. It is thought to occur due to abnormal pressure or mechanical stress chronically applied to the foot, usually with concomitant predisposing conditions such as peripheral sensory neuropathy, peripheral motor neuropathy, autonomic neuropathy or peripheral arterial disease. It is a major complication of diabetes mellitus, and it is a type of diabetic foot disease. Secondary complications to the ulcer, such as infection of the skin or subcutaneous tissue, bone infection, gangrene or sepsis are possible, often leading to amputation.
The periwound is tissue surrounding a wound. Periwound area is traditionally limited to 4 cm outside the wound's edge but can extend beyond this limit if outward damage to the skin is present. Periwound assessment is an important step of wound assessment before wound treatment is prescribed.
References
- ↑ Schultz, GS; Sibbald, RG; Falanga, V; Ayello, EA; Dowsett, C; Harding, K; Romanelli, M; Stacey, MC; Teot, L; Vanscheidt, W (March 2003). "Wound bed preparation: a systematic approach to wound management". Wound Repair and Regeneration. 11 (s1): S1–28. doi:10.1046/j.1524-475X.11.s2.1.x. PMID 12654015. S2CID 25714099.
- ↑ Fletcher, J (April–May 2007). "Wound assessment and the TIME framework". British Journal of Nursing. 16 (8): 462–4, 446. doi:10.12968/bjon.2007.16.8.23415. PMID 17551428.
- ↑ Dowsett, C; Gronemann, M; Harding, K (2015). "Taking wound assessment beyond the edge". Wounds International. 6 (1). Archived from the original on 2018-05-04. Retrieved 2017-06-26.
- ↑ Dowsett, C; Protz, K; Drouard, M; Harding, K (May 2015). "Triangle of wound assessment made easy" (PDF). Wounds International.[ permanent dead link ]
- ↑ Lawton, S; Langøen, A (October 2009). "Assessing and managing vulnerable periwound skin". World Wide Wounds. SMTL. Retrieved May 9, 2017.
- ↑ Cornforth, A (December 2013). "Holistic wound assessment in primary care". British Journal of Community Nursing. 18 (12): S28, S30, S32–4. doi:10.12968/bjcn.2013.18.Sup12.S28. PMID 24796082.
- ↑ Ackermann, PW; Hart, DA (October 2013). "Influence of Comorbidities: Neuropathy, Vasculopathy, and Diabetes on Healing Response Quality". Advances in Wound Care. 2 (8): 410–421. doi:10.1089/wound.2012.0437. PMC 3842870 . PMID 24688829.
- ↑ Anderson, K; Hamm, R (December 2012). "Factors That Impair Wound Healing". Advances in Wound Care. 4 (4): 84–91. doi:10.1016/j.jccw.2014.03.001. PMC 4495737 . PMID 26199879.
- 1 2 Guo, S; Dipietro, LA (March 2010). "Factors affecting wound healing". Journal of Dental Research. 89 (3): 219–29. doi:10.1177/0022034509359125. PMC 2903966 . PMID 20139336.
- ↑ Gosain, A; Dipietro, L (March 2004). "Aging and wound healing". World Journal of Surgery. 28 (3): 321–6. doi:10.1007/s00268-003-7397-6. PMID 14961191.
- ↑ Wilson, JA; Clark, JJ (April–June 2003). "Obesity: impediment to wound healing". Critical Care Nursing Quarterly. 26 (2): 119–32. doi:10.1097/00002727-200304000-00006. PMID 12744592.
- ↑ Arnold, M; Barbul, A (June 2006). "Nutrition and wound healing". Plastic & Reconstructive Surgery. 117 (7S): 42S–58S. doi:10.1097/01.prs.0000225432.17501.6c. PMID 16799374.
- ↑ Russell, L (March 2001). "The importance of patients' nutritional status in wound healing". British Journal of Nursing. 10 (6S): S42, S44–9. doi:10.12968/bjon.2001.10.Sup1.5336. PMID 12070399.
- ↑ "Drugs that delay wound healing". Prescrire International. 22 (137): 94–8. April 2013. PMID 23662318.
- ↑ Silverstein, P (July 1992). "Smoking and wound healing". American Journal of Medicine. 93 (1A): 22S–24S. doi:10.1016/0002-9343(92)90623-J. PMID 1323208.
- ↑ Finnie, A; Nicolson, P (March 2002). "Injecting drug use: implications for skin and wound management". British Journal of Nursing. 11 (6S): S17–28. doi:10.12968/bjon.2002.11.Sup1.12246. PMID 11979188.
- ↑ Price, P; Krasner, DL (August 2014). "Health-related quality of life & chronic wounds". Today's Wound Clinic. 8 (6).
- ↑ Faria, E; Blanes, L; Hochman, B; Filho, MM; Ferreira, L (January 2011). "Health-related quality of life, self-esteem, and functional status of patients with leg ulcers". Wounds: A Compendium of Clinical Research and Practice. 23 (1).
- ↑ Herber, OR; Schnepp, W; Rieger, MA (July 2007). "A systematic review on the impact of leg ulceration on patients' quality of life". Health and Quality of Life Outcomes. 5: 44. doi: 10.1186/1477-7525-5-44 . PMC 1947954 . PMID 17651490.
- ↑ Frykberg, RG; Banks, J (September 2015). "Challenges in the treatment of chronic wounds". Advances in Wound Care. 4 (9): 560–582. doi:10.1089/wound.2015.0635. PMC 4528992 . PMID 26339534.
- ↑ Nicks, BA; Ayello, EA; Woo, K; Nitzki-George, D; Sibbald, RG (December 2010). "Acute wound management: revisiting the approach to assessment, irrigation, and closure considerations". International Journal of Emergency Medicine. 3 (4): 399–407. doi:10.1007/s12245-010-0217-5. PMC 3047833 . PMID 21373312.
- ↑ Benbow, M (March 2016). "Best practice in wound assessment". Nursing Standard. 30 (27): 40–7. doi:10.7748/ns.30.27.40.s45. PMID 26932649. S2CID 2256629.
- ↑ Hollinworth, H (October 2009). "Challenges in protecting peri-wound skin". Nursing Standard. 24 (7): 53–4, 56, 58 passim. doi:10.7748/ns2009.10.24.7.53.c7330. PMID 19927560.
- ↑ Woo, KY; Ayello, EA; Sibbald, G. (2009). "The skin and periwound skin disorders and management". Wound Healing Southern Africa. 2 (2).