Carpal tunnel syndrome (CTS) is the collection of symptoms and signs associated with median neuropathy at the carpal tunnel. Most CTS is related to idiopathic compression of the median nerve as it travels through the wrist at the carpal tunnel (IMNCT). Idiopathic means that there is no other disease process contributing to pressure on the nerve. As with most structural issues, it occurs in both hands, and the strongest risk factor is genetics.

Arthroscopy is a minimally invasive surgical procedure on a joint in which an examination and sometimes treatment of damage is performed using an arthroscope, an endoscope that is inserted into the joint through a small incision. Arthroscopic procedures can be performed during ACL reconstruction.

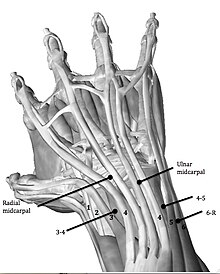
In human anatomy, the wrist is variously defined as (1) the carpus or carpal bones, the complex of eight bones forming the proximal skeletal segment of the hand; (2) the wrist joint or radiocarpal joint, the joint between the radius and the carpus and; (3) the anatomical region surrounding the carpus including the distal parts of the bones of the forearm and the proximal parts of the metacarpus or five metacarpal bones and the series of joints between these bones, thus referred to as wrist joints. This region also includes the carpal tunnel, the anatomical snuff box, bracelet lines, the flexor retinaculum, and the extensor retinaculum.

A ganglion cyst is a fluid-filled bump associated with a joint or tendon sheath. It most often occurs at the back of the wrist, followed by the front of the wrist.

Orthopedic surgery or orthopedics is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors, and congenital disorders.

The Maisonneuve fracture is a spiral fracture of the proximal third of the fibula associated with a tear of the distal tibiofibular syndesmosis and the interosseous membrane. There is an associated fracture of the medial malleolus or rupture of the deep deltoid ligament of the ankle. This type of injury can be difficult to detect.

A distal radius fracture, also known as wrist fracture, is a break of the part of the radius bone which is close to the wrist. Symptoms include pain, bruising, and rapid-onset swelling. The ulna bone may also be broken.

The Galeazzi fracture is a fracture of the distal third of the radius with dislocation of the distal radioulnar joint. It classically involves an isolated fracture of the junction of the distal third and middle third of the radius with associated subluxation or dislocation of the distal radio-ulnar joint; the injury disrupts the forearm axis joint.

Madelung's deformity is usually characterized by malformed wrists and wrist bones and is often associated with Léri-Weill dyschondrosteosis. It can be bilateral or just in the one wrist. It has only been recognized within the past hundred years. Named after Otto Wilhelm Madelung (1846–1926), a German surgeon, who described it in detail, it was noted by others. Guillaume Dupuytren mentioned it in 1834, Auguste Nélaton in 1847, and Joseph-François Malgaigne in 1855.

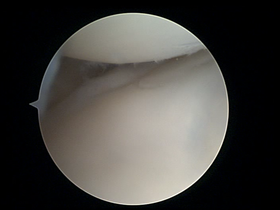
The triangular fibrocartilage complex (TFCC) is formed by the triangular fibrocartilage discus (TFC), the radioulnar ligaments (RULs) and the ulnocarpal ligaments (UCLs).
Shoulder surgery is a means of treating injured shoulders. Many surgeries have been developed to repair the muscles, connective tissue, or damaged joints that can arise from traumatic or overuse injuries to the shoulder.
Microfracture surgery is an articular cartilage repair surgical technique that works by creating tiny fractures in the underlying bone. This causes new cartilage to develop from a so-called super-clot.

Jammed finger is a colloquialism referring to a variety of injuries to the joints of the fingers, resulting from axial loading beyond that which the ligaments can withstand. Common parts of the finger susceptible to this type of injury are ligaments, joints, and bones. The severity of the damage to the finger increases with the magnitude of the force exerted by the external object on the fingertip. Toes may become jammed as well, with similar results.

Radial tunnel syndrome (RTS) is caused by increased pressure on the radial nerve as it travels from the upper arm to the hand and wrist.

The scapholunate ligament is a ligament of the wrist.

Hip arthroscopy refers to the viewing of the interior of the acetabulofemoral (hip) joint through an arthroscope and the treatment of hip pathology through a minimally invasive approach. This technique is sometimes used to help in the treatment of various joint disorders and has gained popularity because of the small incisions used and shorter recovery times when compared with conventional surgical techniques. Hip arthroscopy was not feasible until recently, new technology in both the tools used and the ability to distract the hip joint has led to a recent surge in the ability to do hip arthroscopy and the popularity of it.
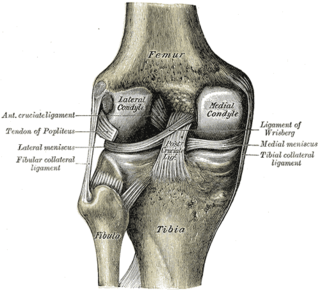
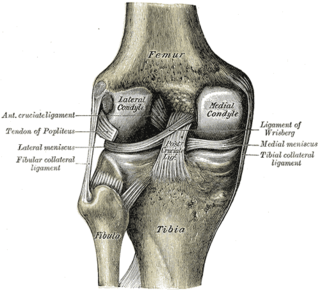
Posterolateral corner injuries of the knee are injuries to a complex area formed by the interaction of multiple structures. Injuries to the posterolateral corner can be debilitating to the person and require recognition and treatment to avoid long term consequences. Injuries to the PLC often occur in combination with other ligamentous injuries to the knee; most commonly the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). As with any injury, an understanding of the anatomy and functional interactions of the posterolateral corner is important to diagnosing and treating the injury.

Wrist osteoarthritis is gradual loss of articular cartilage and hypertrophic bone changes (osteophytes). While in many joints this is part of normal aging (senescence), in the wrist osteoarthritis usually occurs over years to decades after scapholunate interosseous ligament rupture or an unhealed fracture of the scaphoid. Characteristic symptoms including pain, deformity and stiffness. Pain intensity and incapability are notably variable and do not correspond with arthritis severity on radiographs.

Lister's tubercle or dorsal tubercle of radius is a bony prominence located at the distal end of the radius. It is palpable on the dorsum of the wrist.

Labral reconstruction is a type of hip arthroscopy in which the patient's native labrum is partially or completely removed and reconstructed using either autograft or allograft tissue. Originally described in 2009 using the ligamentum teres capitis, arthroscopic labral reconstruction using a variety of graft tissue has demonstrated promising short and mid-term clinical outcomes. Most importantly, labral reconstruction has demonstrated utility when the patient's native labral tissue is far too damaged for debridement or repair.