A cyst, also traditionally known from Old English as a wen, is a closed sac, having a distinct envelope and division compared with the nearby tissue. Hence, it is a cluster of cells that have grouped together to form a sac ; however, the distinguishing aspect of a cyst is that the cells forming the "shell" of such a sac are distinctly abnormal when compared with all surrounding cells for that given location. A cyst may contain air, fluids, or semi-solid material. A collection of pus is called an abscess, not a cyst. Once formed, a cyst may resolve on its own. When a cyst fails to resolve, it may need to be removed surgically, but that would depend upon its type and location.

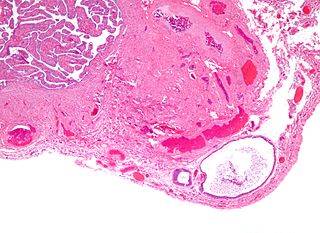
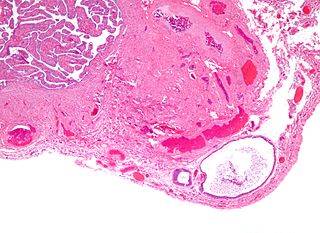
A hydrocele testis is an accumulation of clear fluid within the cavum vaginale, the potential space between the layers of the tunica vaginalis of the testicle. It is the most common form of hydrocele and is often referred to simply as a "hydrocele". A primary hydrocele testis causes a painless enlargement in the scrotum on the affected side and is thought to be due to the defective absorption of fluid secreted between the two layers of the tunica vaginalis. A secondary hydrocele is secondary to either inflammation or a neoplasm in the testis.

An adenoma is a benign tumor of epithelial tissue with glandular origin, glandular characteristics, or both. Adenomas can grow from many glandular organs, including the adrenal glands, pituitary gland, thyroid, prostate, and others. Some adenomas grow from epithelial tissue in nonglandular areas but express glandular tissue structure. Although adenomas are benign, they should be treated as pre-cancerous. Over time adenomas may transform to become malignant, at which point they are called adenocarcinomas. Most adenomas do not transform. However, even though benign, they have the potential to cause serious health complications by compressing other structures and by producing large amounts of hormones in an unregulated, non-feedback-dependent manner. Some adenomas are too small to be seen macroscopically but can still cause clinical symptoms.
In medical or research imaging, an incidental imaging finding is an unanticipated finding which is not related to the original diagnostic inquiry. As with other types of incidental medical findings, they may represent a diagnostic, ethical, and philosophical dilemma because their significance is unclear. While some coincidental findings may lead to beneficial diagnoses, others may lead to overdiagnosis that results in unnecessary testing and treatment, sometimes called the "cascade effect".

Sex cord–gonadal stromal tumour is a group of tumors derived from the stromal component of the ovary and testis, which comprises the granulosa, thecal cells and fibrocytes. In contrast, the epithelial cells originate from the outer epithelial lining surrounding the gonad while the germ cell tumors arise from the precursor cells of the gametes, hence the name germ cell. In humans, this group accounts for 8% of ovarian cancers and under 5% of testicular cancers. Their diagnosis is histological: only a biopsy of the tumour can make an exact diagnosis. They are often suspected of being malignant prior to operation, being solid ovarian tumours that tend to occur most commonly in post menopausal women.

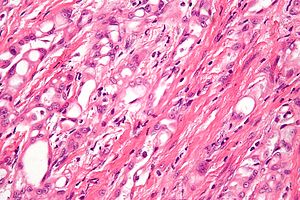
Fibroadenomas are benign breast tumours characterized by an admixture of stromal and epithelial tissue. Breasts are made of lobules and ducts. These are surrounded by glandular, fibrous and fatty tissues. Fibroadenomas develop from the lobules. The glandular tissue and ducts grow over the lobule to form a solid lump.

A hematocele is a collections of blood in a body cavity or potential space. The term most commonly refers to the collection of blood in the tunica vaginalis around the testes, known as a scrotal hematocele. Hematoceles can also occur in the abdominal cavity and other body cavities. Hematoceles are rare, making them harder to diagnose and treat. They are very common especially as slowly growing masses in the scrotum usually in men older than 50 years.

A seminoma is a germ cell tumor of the testicle or, more rarely, the mediastinum or other extra-gonadal locations. It is a malignant neoplasm and is one of the most treatable and curable cancers, with a survival rate above 95% if discovered in early stages.

Pleomorphic adenoma is a common benign salivary gland neoplasm characterised by neoplastic proliferation of epithelial (ductal) cells along with myoepithelial components, having a malignant potentiality. It is the most common type of salivary gland tumor and the most common tumor of the parotid gland. It derives its name from the architectural Pleomorphism seen by light microscopy. It is also known as "Mixed tumor, salivary gland type", which refers to its dual origin from epithelial and myoepithelial elements as opposed to its pleomorphic appearance.

Calretinin, also known as calbindin 2, is a calcium-binding protein involved in calcium signaling. In humans, the calretinin protein is encoded by the CALB2 gene.

Adrenocortical adenoma is commonly described as a benign neoplasm emerging from the cells that comprise the adrenal cortex. Like most adenomas, the adrenocortical adenoma is considered a benign tumor since the majority of them are non-functioning and asymptomatic. Adrenocortical adenomas are classified as ACTH-independent disorders, and are commonly associated with conditions linked to hyperadrenalism such as Cushing's syndrome (hypercortisolism) or Conn's syndrome (hyperaldosteronism), which is also known as primary aldosteronism. In addition, recent case reports further support the affiliation of adrenocortical adenomas with hyperandrogenism or florid hyperandrogenism which can cause hyperandrogenic hirsutism in females. "Cushing's syndrome" differs from the "Cushing's disease" even though both conditions are induced by hypercortisolism. The term "Cushing's disease" refers specifically to "secondary hypercortisolism" classified as "ACTH-dependent Cushing's syndrome" caused by pituitary adenomas. In contrast, "Cushing's syndrome" refers specifically to "primary hypercortisolism" classified as "ACTH-independent Cushing's syndrome" caused by adrenal adenomas.
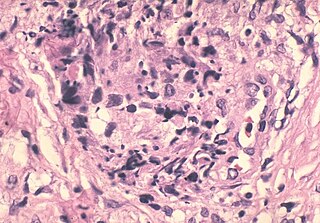
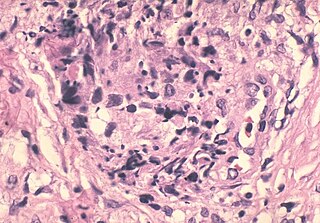
A sperm granuloma is a lump of leaked sperm that appears along the vasa deferentia or epididymides in vasectomized individuals. While the majority of sperm granulomas are present along the vas deferens, the rest of them form at the epididymis. Sperm granulomas range in size, from one millimeter to one centimeter. They consist of a central mass of degenerating sperm surrounded by tissue containing blood vessels and immune system cells. Sperm granulomas may also have a yellow, white, or cream colored center when cut open. While some sperm granulomas can be painful, most of them are painless and asymptomatic. Sperm granulomas can appear as a result of surgery, trauma, or an infection. They can appear as early as four days after surgery and fully formed ones can appear as late as 208 days later.

Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
Walthard cell rests, sometimes called Walthard cell nests, are a benign cluster of epithelial cells most commonly found in the connective tissue of the Fallopian tubes, but also seen in the mesovarium, mesosalpinx and ovarian hilus.

Myelolipoma is a benign tumor-like lesion composed of mature adipose (fat) tissue and haematopoietic (blood-forming) elements in various proportions.

A Sertoli cell tumour, also Sertoli cell tumor, is a sex cord–gonadal stromal tumour of Sertoli cells. They can occur in the testis or ovary. They are very rare and generally peak between the ages of 35 and 50. They are typically well-differentiated, and may be misdiagnosed as seminomas as they often appear very similar.
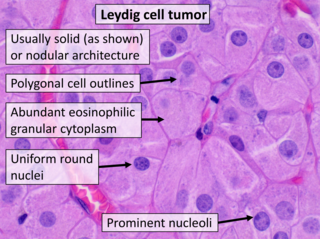
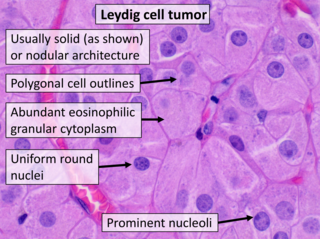
Leydig cell tumour, also Leydig cell tumor, (testicular) interstitial cell tumour and (testicular) interstitial cell tumor, is a member of the sex cord-stromal tumour group of ovarian and testicular cancers. It arises from Leydig cells. While the tumour can occur at any age, it occurs most often in young adults.

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.
Male genital examination is a physical examination of the genital in males to detect ailments and to assess sexual development and is normally included in an annual physical examination. The examination includes checking the penis, scrotum, and urethral meatus. A comprehensive assessment of the male genitals assesses the pubic hair based on Sexual Maturity Rating and the size of the testicles and penis. The exam is conducted to detect various ailments, measure sexual development, or verify a person's age and biological sex. The genitourinary system can also be assessed as part of the male genital examination. During a genital examination, the doctor can detect any of the following: structural abnormalities, urethral opening abnormalities, problems related to uncircumcision, lumps, tumors, redness, excoriation, edema, lesions, swelling, cancer, hair-related issues and many others. In some instances where a physical examination of the male genitals is not sufficient to diagnose an individual than an internal genital examination using imaging or ultrasounds will be needed for further evaluation.

Vaginal cysts are uncommon benign cysts that develop in the vaginal wall. The type of epithelial tissue lining a cyst is used to classify these growths. They can be congenital. They can present in childhood and adulthood. The most common type is the squamous inclusion cyst. It develops within vaginal tissue present at the site of an episiotomy or other vaginal surgical sites. In most instances they do not cause symptoms and present with few or no complications. A vaginal cyst can develop on the surface of the vaginal epithelium or in deeper layers. Often, they are found by the woman herself and as an incidental finding during a routine pelvic examination. Vaginal cysts can mimic other structures that protrude from the vagina such as a rectocele and cystocele. Some cysts can be distinguished visually but most will need a biopsy to determine the type. Vaginal cysts can vary in size and can grow as large as 7 cm. Other cysts can be present on the vaginal wall though mostly these can be differentiated. Vaginal cysts can often be palpated (felt) by a clinician. Vaginal cysts are one type of vaginal mass, others include cancers and tumors. The prevalence of vaginal cysts is uncertain since many go unreported but it is estimated that 1 out of 200 women have a vaginal cyst. Vaginal cysts may initially be discovered during pregnancy and childbirth. These are then treated to provide an unobstructed delivery of the infant. Growths that originate from the urethra and other tissue can present as cysts of the vagina.