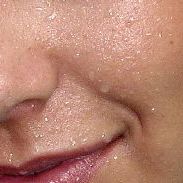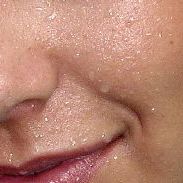
Perspiration, also known as sweat, is the fluid secreted by sweat glands in the skin of mammals.

Hematidrosis, also called hematohidrosis, haematidrosis, hemidrosis and blood sweat, is a very rare condition in which a human sweats blood. The term is from Ancient Greek haîma/haímatos, meaning blood, and hīdrṓs, meaning sweat.

Hives, also known as urticaria, is a kind of skin rash with red and/or flesh-colored, raised, itchy bumps. Hives may burn or sting. The patches of rash may appear on different body parts, with variable duration from minutes to days, and do not leave any long-lasting skin change. Fewer than 5% of cases last for more than six weeks. The condition frequently recurs.

Miliaria, commonly known as heat rash, sweat rash, or prickly heat, is a skin disease marked by small, itchy rashes due to sweat trapped under the skin by clogged sweat-gland ducts. Miliaria is a common ailment in hot and humid conditions, such as in the tropics and during the summer. Although it affects people of all ages, it is especially common in children and infants due to their underdeveloped sweat glands.

Cold urticaria is a disorder in which large red welts called hives (urticaria) form on the skin after exposure to a cold stimulus. The hives are usually itchy and often the hands, feet and other parts of the body will become itchy and swollen as well. Hives vary in size from about 7 mm in diameter to as big as about 27 mm or larger.

Dermatographic urticaria is a skin disorder and one of the most common types of urticaria, affecting 2–5% of the population.
Aquagenic pruritus is a skin condition characterized by the development of severe, intense, prickling-like epidermal itching without observable skin lesions and evoked by contact with water.

Urticaria pigmentosa (also known as generalized eruption of cutaneous mastocytosis (childhood type) ) is the most common form of cutaneous mastocytosis. It is a rare disease caused by excessive numbers of mast cells in the skin that produce hives or lesions on the skin when irritated.

Physical urticaria is a distinct subgroup of urticaria (hives) that are induced by an exogenous physical stimulus rather than occurring spontaneously. There are seven subcategories that are recognized as independent diseases. Physical urticaria is known to be painful, itchy and physically unappealing; it can recur for months to years.

CCL17 is a powerful chemokine produced in the thymus and by antigen-presenting cells like dendritic cells, macrophages, and monocytes. CCL17 plays a complex role in cancer. It attracts T-regulatory cells allowing for some cancers to evade an immune response. However, in other cancers, such as melanoma, an increase in CCL17 is linked to an improved outcome. CCL17 has also been linked to autoimmune and allergic diseases.

Pitted keratolysis is a bacterial skin infection of the foot. The infection is characterized by craterlike pits on the sole of the feet and toes, particularly weight-bearing areas.
Hypohidrosis is a medical condition in which a person exhibits diminished sweating in response to appropriate stimuli. In contrast with hyperhidrosis, which is a socially troubling yet often benign condition, the consequences of untreated hypohidrosis include hyperthermia, heat stroke and death. An extreme case of hypohidrosis in which there is a complete absence of sweating and the skin is dry is termed anhidrosis. The condition is also known as adiaphoresis, ischidrosis, oligidria, oligohidrosis and sweating deficiency.

Solar urticaria (SU) is a rare condition in which exposure to ultraviolet or UV radiation, or sometimes even visible light, induces a case of urticaria or hives that can appear in both covered and uncovered areas of the skin. It is classified as a type of physical urticaria. The classification of disease types is somewhat controversial. One classification system distinguished various types of SU based on the wavelength of the radiation that causes the breakout; another classification system is based on the type of allergen that initiates a breakout.
Aquagenic urticaria, also known as water allergy and water urticaria, is a form of physical urticaria in which hives develop on the skin after contact with water, regardless of its temperature. The condition typically results from contact with water of any type, temperature or additive.
Ross' syndrome consists of Adie's syndrome plus segmental anhidrosis.
Idiopathic pure sudomotor failure (IPSF) is the most common cause of a rare disorder known as acquired idiopathic generalized anhidrosis (AIGA), a clinical syndrome characterized by generalized decrease or absence of sweating without other autonomic and somatic nervous dysfunctions and without persistent organic cutaneous lesions.
Acquired idiopathic generalized anhidrosis (AIGA) is characterized by generalized absence of sweating without other autonomic and neurologic dysfunction. Other symptoms include facial flushing, headaches, disorientation, lassitude, hyperthermia, weakness, and palpitations.

Chronic spontaneous urticaria(CSU) also known as Chronic idiopathic urticaria(CIU) is defined by the presence of wheals, angioedema, or both for more than six weeks. The most common symptoms of chronic spontaneous urticaria are angioedema and hives that are accompanied by itchiness.
A sweat allergy is the exacerbation of atopic dermatitis associated with an elevated body temperature and resulting increases in the production of sweat. It appears as small reddish welts that become visible in response to increased temperature and resulting production of sweat. It can affect all ages. Sweating can trigger intense itching or cholinergic urticaria. The protein MGL_1304 secreted by mycobiota (fungi) present on the skin such as Malassezia globosa acts as a histamine or antigen. People can be desensitized using their own samples of sweat that have been purified that contains small amounts of the allergen. The allergy is not due to the sweat itself but instead to an allergy-producing protein secreted by microorganisms found on the skin.

Autoimmune urticaria, also known as chronic autoimmune urticaria, is a type of chronic urticaria characterized by the presence of autoantibodies in the patient's immune system that target the body's own mast cells, leading to episodes of hives (urticaria). This immunologically distinct type of urticaria is considered autoimmune because the immune system, which normally protects the body from foreign organisms, mistakenly attacks the body's own cells, causing inflammation and other symptoms.